Treatment options for kidney stones

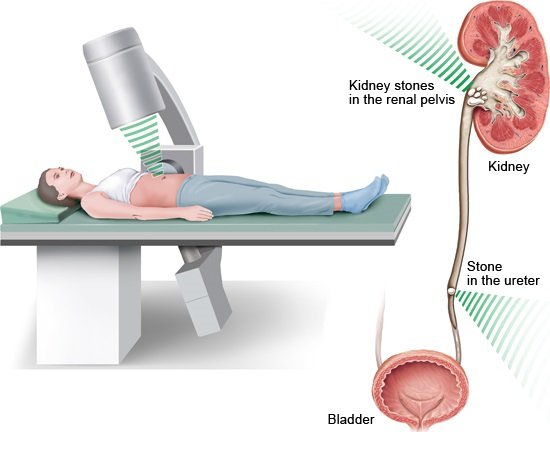
Small kidney stones often pass out of the body on their own. As long as they don't cause severe pain or complications, treatment isn’t necessary. Larger kidney stones usually need to be treated. Depending on how large the kidney stones are and where they're located, they can be destroyed or removed using an endoscope (a flexible tube with a light and camera at the end of it).
Most kidney stones with a diameter of less than 5 millimeters, and about half of all stones between 5 and 10 millimeters, pass out of the body on their own. These smaller kidney stones are often flushed out in the urine after one or two weeks.
If it’s thought that a stone will probably be flushed out without any treatment, doctors generally recommend waiting. If the kidney stone causes pain as it travels through the ureter (tube that runs from a kidney to the bladder), painkillers like ibuprofen or diclofenac can provide relief.
Larger stones that cause problems will usually have to be broken up or surgically removed. That needs to be done if
- the stone isn't passed within four weeks,
- there are complications,
- it causes severe colic (pain), or
- the stone is larger than 10 millimeters in diameter.
Uric acid stones can sometimes be dissolved using medication.