Scabies: How can you prevent infection?

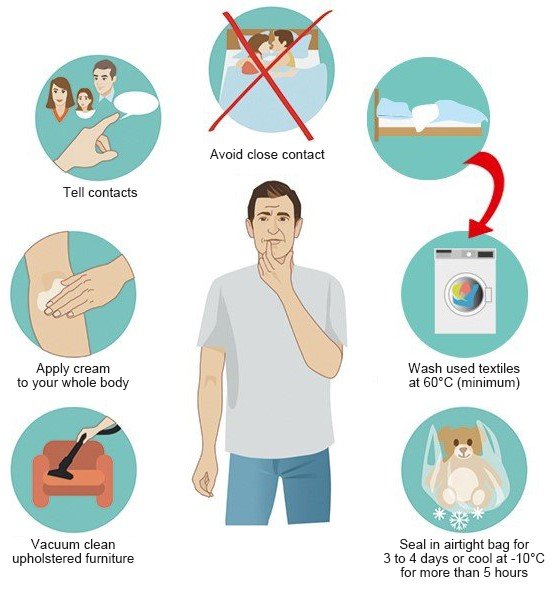
There is no need to take special measures to prevent scabies in everyday life. But if you're infected with scabies, it's important that you protect others and also make sure that you don't become infected again yourself after treatment.
Scabies causes itching, particularly at night. Other symptoms may include small red patches of skin, raised lines, a rash with little bumps as well as areas that have been scratched open. But these symptoms usually only start to show about two to five weeks after you are infected.
Because of this, it's important to tell everyone who you may have infected in the meantime. It is also important to avoid close physical contact with other people until you have finished your treatment, and to make sure that you don't become infected again yourself – for instance, through used clothes and bedding.