Spondylolisthesis: Is surgery a good option?

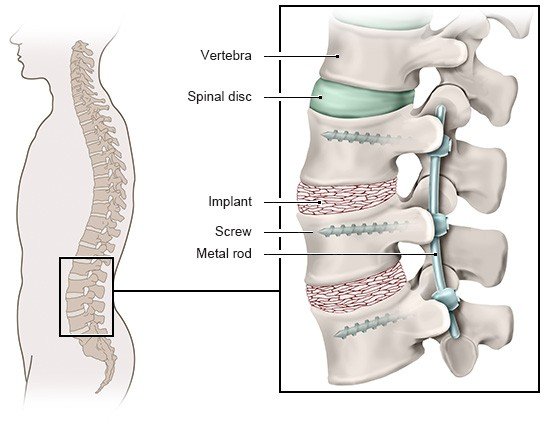
If you’ve had spondylolisthesis symptoms for a long time and they’re making things difficult in your day-to-day life, it might be worth it to consider surgery. There isn’t any proof though that surgery is more effective than conservative (non-surgical) treatment. If you’re not sure, you can ask for a second medical opinion.
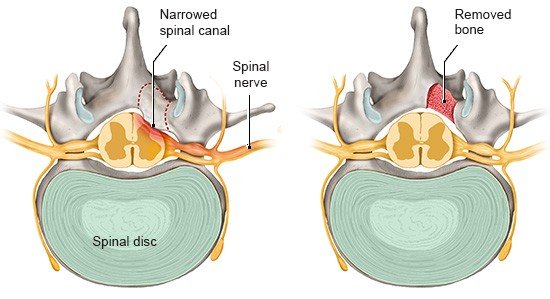
Spondylolisthesis is when vertebrae slide against each other. It tends to happen around the lower spine (lumbar region). The vertebra that has slipped can make the spinal canal narrower. The spinal cord, nerves and vessels run through this canal. If narrowing in the spinal canal is putting pressure on the nerves, you might feel pain in your back, which can spread to your bottom or legs. Numbness and tingling in the feet or legs are also possible.
Spondylolisthesis is typically treated using conservative methods like physical therapy and painkillers. Surgery isn’t considered unless the symptoms are causing a great deal of distress and other treatments aren’t providing enough relief. There hasn’t been much good-quality research on whether and how much surgery can help. So it’s worth it to take the time to weigh the pros and cons because there are various risks involved when you have surgery on your back. If you’re not sure, you can ask for an independent second opinion from another doctor.