Ammendolia C, Hofkirchner C, Plener J et al. Non-operative treatment for lumbar spinal stenosis with neurogenic claudication: an updated systematic review. BMJ Open 2022; 12(1): e057724.
Ammendolia C, Schneider M, Williams K et al. The physical and psychological impact of neurogenic claudication: the patients' perspectives. J Can Chiropr Assoc 2017; 61(1): 18-31.
Deutsche Gesellschaft für Neurologie (DGN). Lumbale Radikulopathie (S2k-Leitlinie, under revision). AWMF register no.: 030-058. 2018.
Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie (DGOOC). S2k-Leitlinie Spezifischer Kreuzschmerz. AWMF register no.: 187-059. 2024.
Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie (DGOOC), Deutsche Gesellschaft für Orthopädie und Unfallchirurgie (DGOU), Deutsche Gesellschaft für Neurochirurgie (DGNC) et al. Leitlinie zur konservativen, operativen und rehabilitativen Versorgung bei Bandscheibenvorfällen mit radikulärer Symptomatik (S2k-Leitlinie, under revision). AWMF register no.: 033-048. 2020.
Kasch R, Truthmann J, Hancock MJ et al. Association of Lumbar MRI Findings with Current and Future Back Pain in a Population-based Cohort Study. Spine (Phila Pa 1976) 2022; 47(3): 201-211.
Katz JN, Zimmerman ZE, Mass H et al. Diagnosis and Management of Lumbar Spinal Stenosis: A Review. JAMA 2022; 327(17): 1688-1699.
Mancuso CA, Rigaud MC, Wellington B et al. Qualitative assessment of patients' perspectives and willingness to improve healthy lifestyle physical activity after lumbar surgery. Eur Spine J 2021; 30(1): 200-207.
Mayer HM, Heider FC. Der lumbale Bandscheibenvorfall. Orthopädie und Unfallchirurgie up2date 2016; 11(06): 427-447.
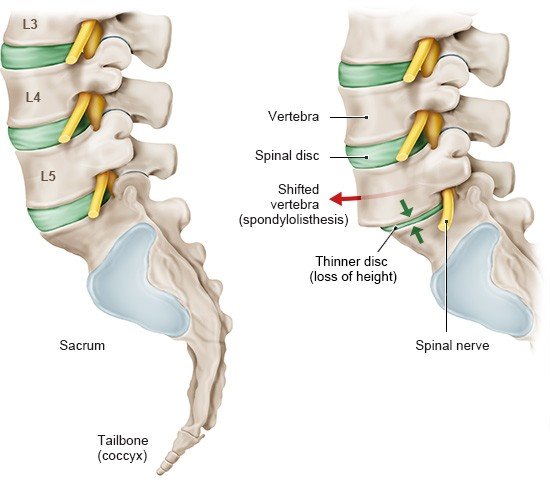
North American Spine Society (NASS). Diagnosis and treatment of adult isthmic spondylolisthesis. (Evidence-Based Clinical Guidelines for Multidisciplinary Spine Care). 2014.
North American Spine Society (NASS). Diagnosis and treatment of degenerative lumbar spondylolisthesis. (Clinical Guidelines for Multidisciplinary Spine Care). 2014.
Rushton A, Jadhakhan F, Masson A et al. Patient journey following lumbar spinal fusion surgery (FuJourn): A multicentre exploration of the immediate post-operative period using qualitative patient diaries. PLoS One 2020; 15(12): e0241931.
Schulte TL, Ringel F, Quante M et al. Surgery for adult spondylolisthesis: a systematic review of the evidence. Eur Spine J 2016; 25(8): 2359-2367.
Van der Horst AY, Trompetter HR, Pakvis DFM et al. Between hope and fear: A qualitative study on perioperative experiences and coping of patients after lumbar fusion surgery. Int J Orthop Trauma Nurs 2019; 35: 100707.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.