Surgery for treating retinal detachment

If the retina has detached, fast surgery is needed to save or improve vision again. There are different procedures for reattaching the retina. Sometimes several procedures are needed.
Retinal detachment is where the retina is no longer in contact with the inside of the eyeball. That’s usually caused by small tears in the retina. The gel-like fluid from the vitreous body can pass through them and collect beneath the retina, meaning the retina is no longer supplied with nutrients from the layer below. That can permanently damage the sensory cells in the retina.
Retinal detachment is a medical emergency, and surgery is usually the only treatment that makes sense. In most people, the retina can then be reattached. That usually means that the affected eye can be prevented from going blind and vision can be improved again.
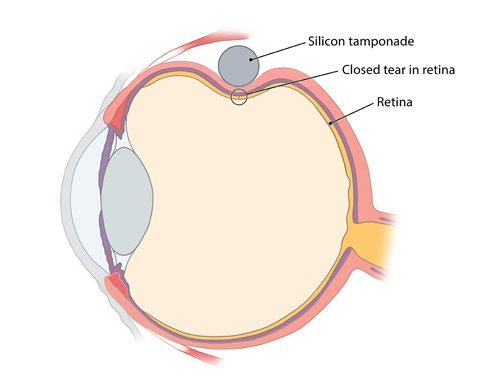
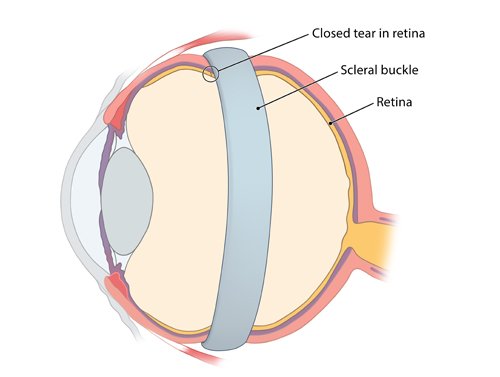
The two most common surgical procedures for reattaching the retina scleral buckling and removal of the vitreous body (vitrectomy). Which procedure makes most sense depends on a number of factors, including the size and the duration of the detachment. Sometimes, both methods are even combined.