Introduction

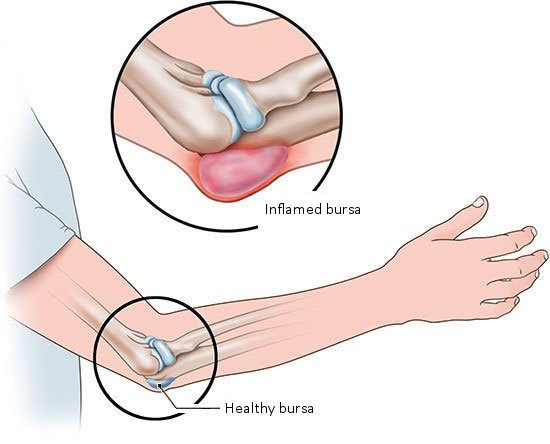
Bursitis is an inflammation in one of the small, fluid-filled sacs (bursae) often found near joints in the body. It can be very painful and limit mobility. The inflammation can result when too much pressure is put on one of these sacs (a bursa).
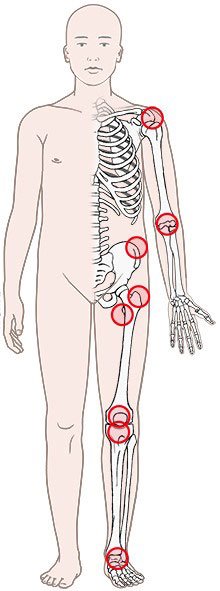
The bursae (Latin for bags) are made of connective tissue and filled with synovial fluid. Like tiny pillows, they cushion parts of the body like the elbows, which are often exposed to friction or pressure. When you prop your elbows on a hard tabletop, the bursa prevents the bone from pressing too hard against your skin. There are over one hundred bursae in the human body, many of them near joints.
Bursitis can also be caused by a – usually bacterial – infection.