Introduction

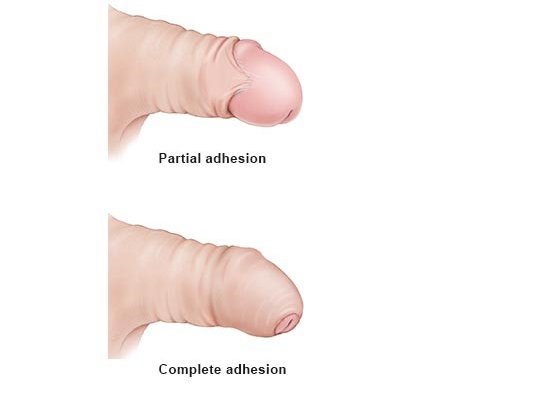
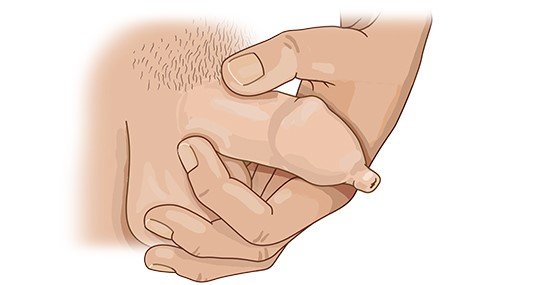
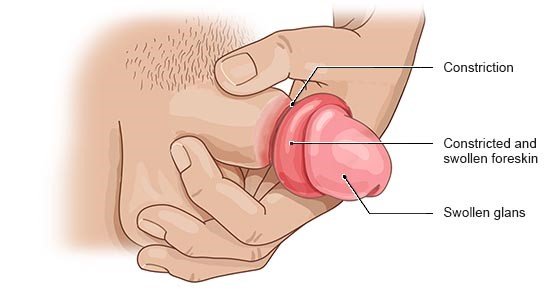
The foreskin is a flap of skin at the tip of the penis that covers the glans (head of the penis). It can be pulled back to uncover the glans. If it can’t be pulled back or if it is painful, doctors refer to the condition as “phimosis.”
It is perfectly normal that in newborns or young boys the foreskin can’t be pulled back. This is not a cause for concern: Nearly all newborn boys have foreskins that are tight or stuck to the head of the glans (adhesion). This natural “phimosis” protects the sensitive head of the penis from rubbing against things, becoming too dry or coming into contact with germs like viruses or bacteria. A tight foreskin should never be forced back. That is painful and may damage the skin.
Within the first few years of life, the stuck skin usually detaches, and tight foreskin usually gradually loosens, making it increasingly easy to pull back without any pain. So it simply takes time. Phimosis should only be treated if it doesn't go away on its own by puberty or if it is causing problems.
Phimosis may also develop in adulthood, sometimes as a complication of inflammation.