What are the treatment options for phimosis?

Nearly all boys have a naturally tightened foreskin for their first several years of life, which than goes away on its own. Treatment is recommended only if it causes problems or remains that way until the child reaches puberty. Using a steroid cream is often enough. Surgery is only rarely needed.
If parents notice that their son’s foreskin can't be pulled back, there is no need for them to worry. It is normal for the foreskin of baby boys and toddlers to be tight or stuck to the head of their penis (glans): Nearly all boys are born with this kind of natural phimosis. It protects the glans and the urethra (urine tube) from things like germs.
Areas of stuck skin (adhesions) usually detach and tight foreskins usually loosen on their own within the first few years of life. So experts recommend first waiting if the child experiences problems like pain or trouble peeing.
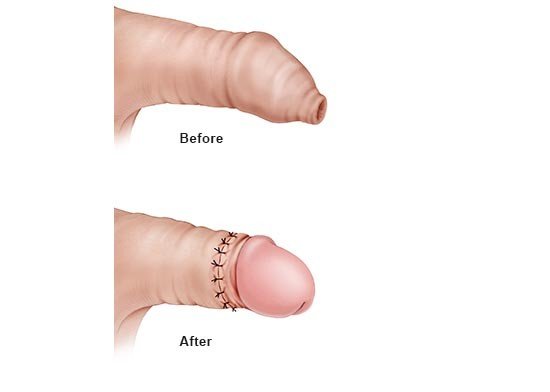
The foreskin only rarely remains tightened into puberty (congenital phimosis). By then it will probably not go away on its own and it’s a good idea to talk with a doctor about treatment, even if the phimosis isn’t causing any problems. Treatment should also be considered if the foreskin first became too tight later in life as the result of scarring (acquired phimosis).