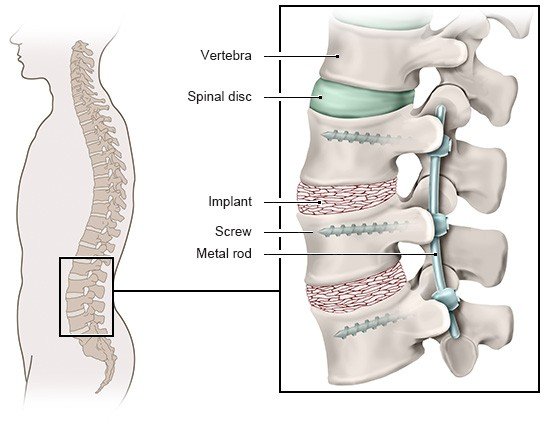
Abdel-Fattah AR, Bell F, Boden L et al. To fuse or not to fuse: The elderly patient with lumbar stenosis and low-grade spondylolisthesis. Systematic review and meta-analysis of randomised controlled trials. Surgeon 2023; 21(1): e23-e31.
Bove AM, Lynch AD, Ammendolia C et al. Patients' experience with nonsurgical treatment for lumbar spinal stenosis: a qualitative study. Spine J 2018; 18(4): 639-647.
Chen Z, Wu W, Xiong H et al. Systematic review and meta-analysis of the therapeutic effects of minimally invasive transforaminal interbody fusion on spondylolisthesis. Ann Palliat Med 2021; 10(9): 9848-9858.
Chen Z, Xie P, Feng F et al. Decompression Alone Versus Decompression and Fusion for Lumbar Degenerative Spondylolisthesis: A Meta-Analysis. World Neurosurg 2018; 111: e165-e177.
Davis RE, Vincent C, Henley A et al. Exploring the care experience of patients undergoing spinal surgery: a qualitative study. J Eval Clin Pract 2013; 19(1): 132-138.
Deutsche Gesellschaft für Neurologie (DGN). Leitlinien für Diagnostik und Therapie in der Neurologie: Lumbale Radikulopathie (S2k-Leitlinie). AWMF register no.: 030-058. 2018.
Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie (DGOOC). Spezifischer Kreuzschmerz (S2k-Leitlinie, in Überarbeitung). AWMF register no.: 187-059. 2017.
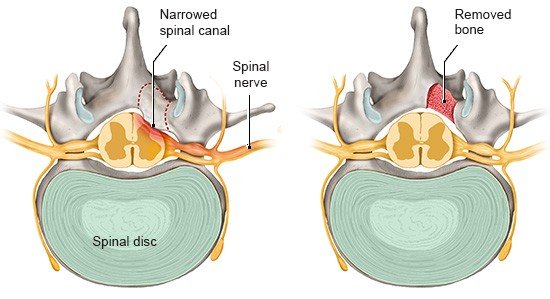
Kalff R, Ewald C, Waschke A et al. Degenerative lumbar spinal stenosis in older people: current treatment options [Degenerative lumbale Spinalkanalstenose im höheren Lebensalter: Aktuelle Behandlungsoptionen]. Dtsch Arztebl 2013; 110(37): 613-624.
Machado GC, Ferreira PH, Yoo RI et al. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev 2016; (11): CD012421.
North American Spine Society. Diagnosis and treatment of degenerative lumbar spinal stenosis. 2011.
Peterson S, Mesa A, Halpert B et al. How people with lumbar spinal stenosis make decisions about treatment: A qualitative study using the Health Belief Model. Musculoskelet Sci Pract 2021; 54: 102383.
Pranata R, Lim MA, Vania R et al. Decompression Alone Compared to Decompression With Fusion in Patients With Lumbar Spondylolisthesis: Systematic Review, Meta-Analysis, and Meta-Regression. Int J Spine Surg 2022; 16(1): 71-80.
Thomé C, Börm W, Meyer F. Degenerative lumbar spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int 2008; 105(20): 373-379.
Zaina F, Tomkins-Lane C, Carragee E et al. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev 2016; (1): CD010264.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.