Advantages and disadvantages of screening tests

This information offers a detailed description of the advantages and disadvantages of screening. It also explains why research is needed to be able to say which tests are beneficial and which are harmful.
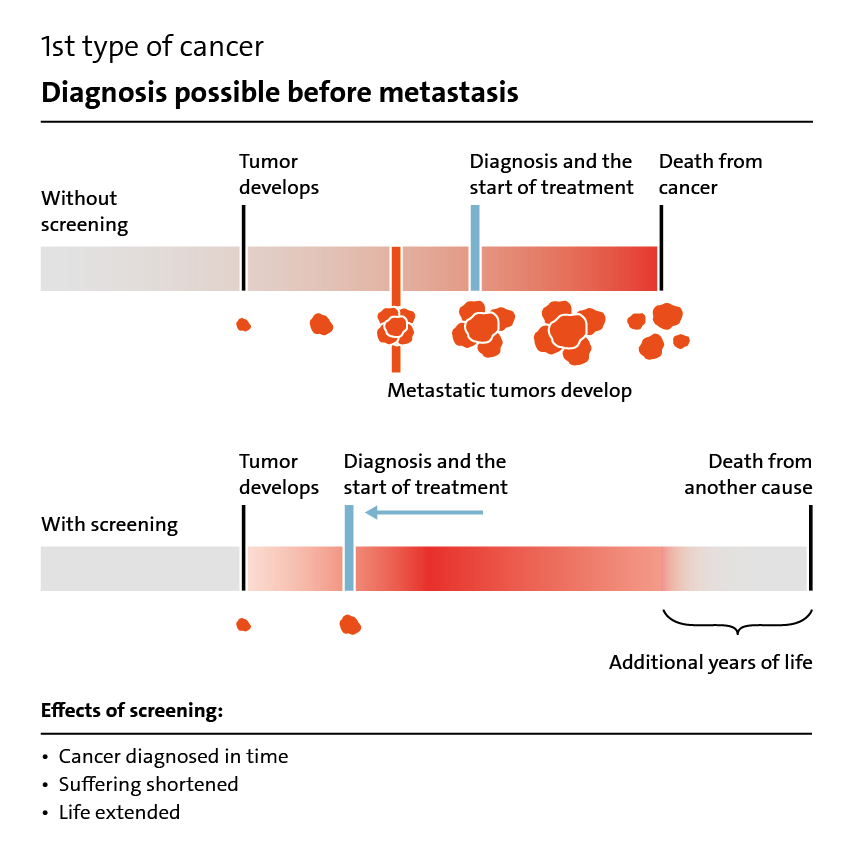
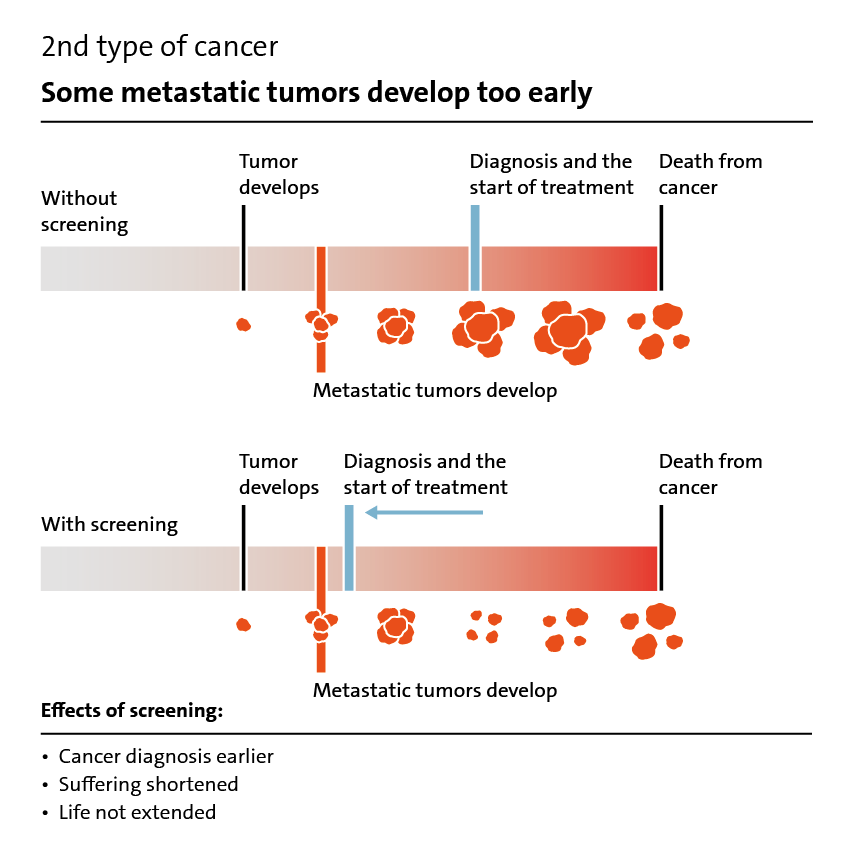
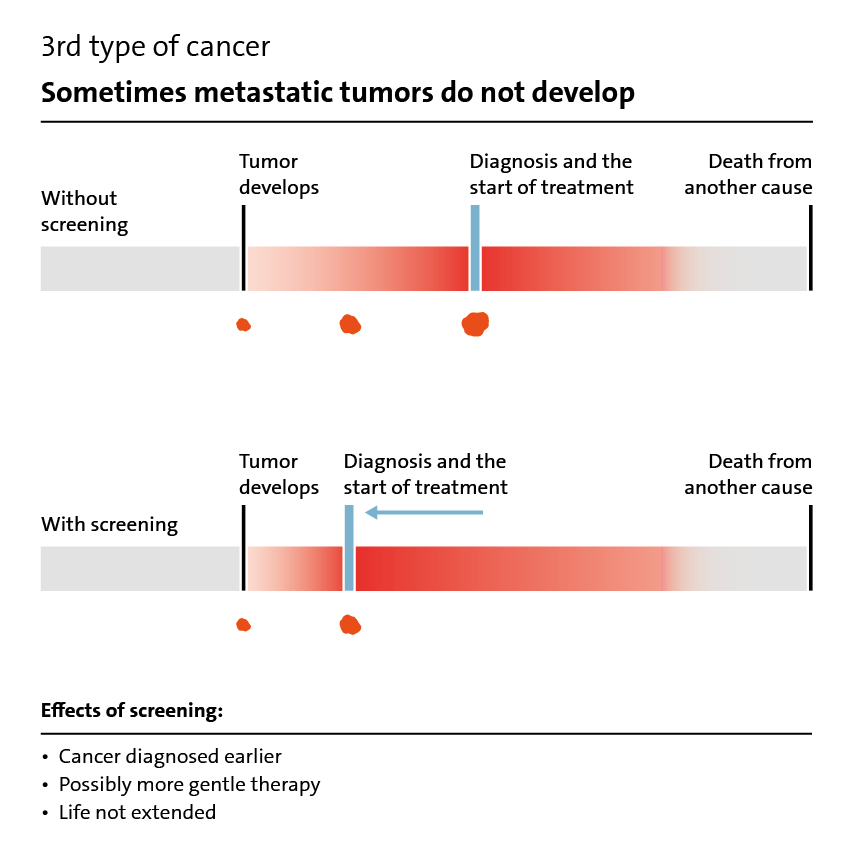
Medical tests are usually done to find out what is causing certain symptoms. Screening tests are different: they are done in people without any symptoms. They are designed to detect diseases as early as possible so that they can be treated effectively or, ideally, cured. The idea makes perfect sense on the face of it. Certain tests, like colonoscopies, can also detect cancer in its earliest stages, enabling it to be removed. Screening tests that stop a disease from developing are called “preventive testing.”
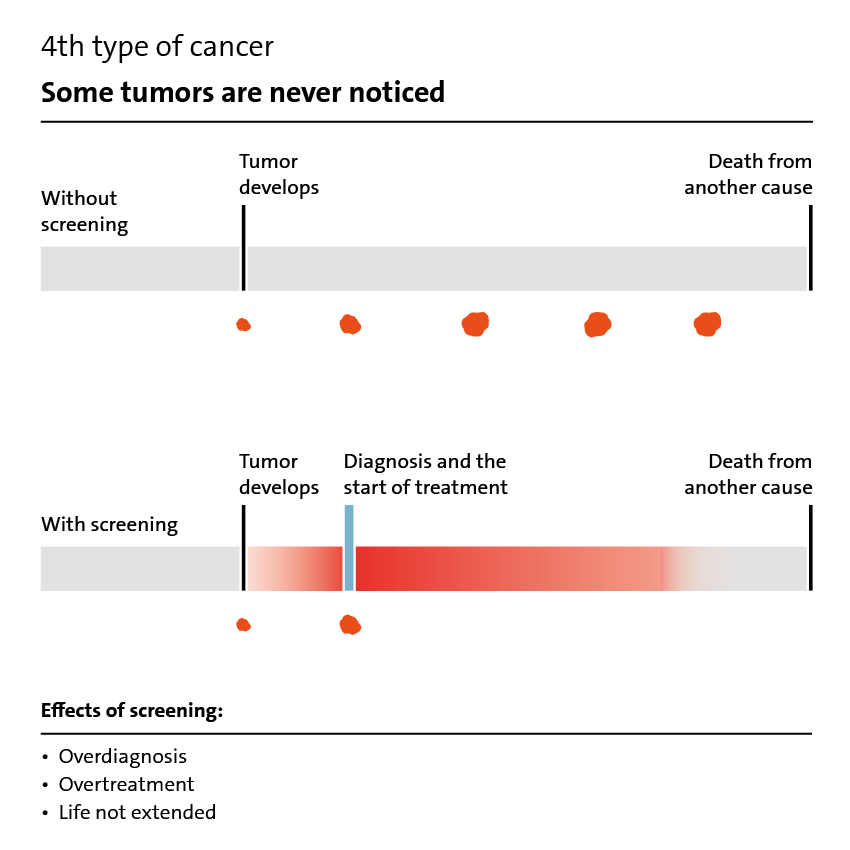
But screening doesn‘t always stop disease. One example of this is screening for ovarian cancer. This often involves an ultrasound scan, which doesn’t improve the person‘s chances of recovery. Screening for other diseases, such as prostate cancer, does have advantages but there are serious disadvantages too.
A few simple questions can help you work out which tests you want and which ones you don‘t think you need. This information offers a detailed description of the advantages and disadvantages of screening. It also explains why research is needed to be able to say which tests are beneficial and which are harmful.