The breast cancer screening program in Germany

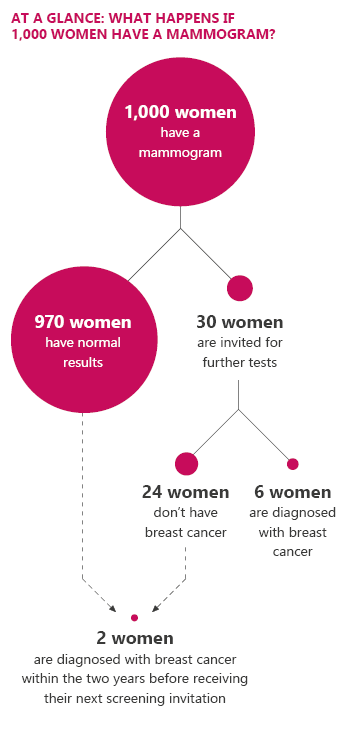
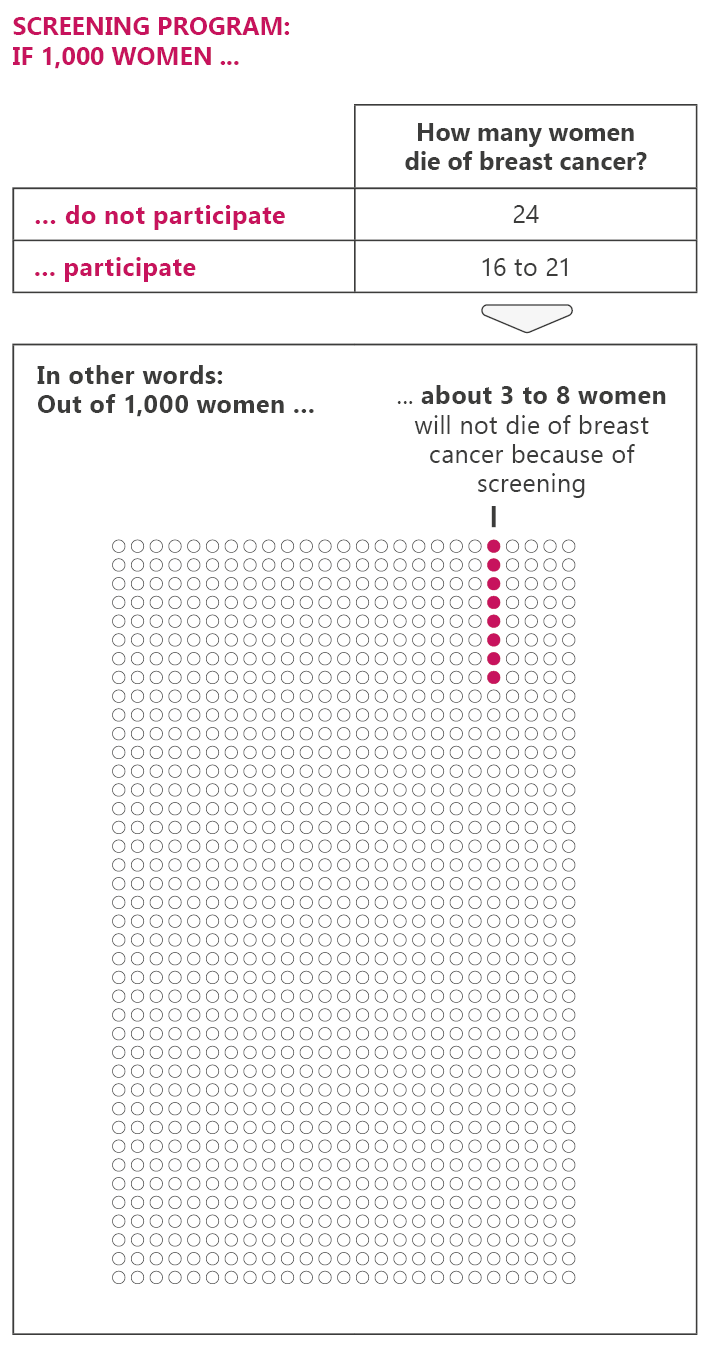
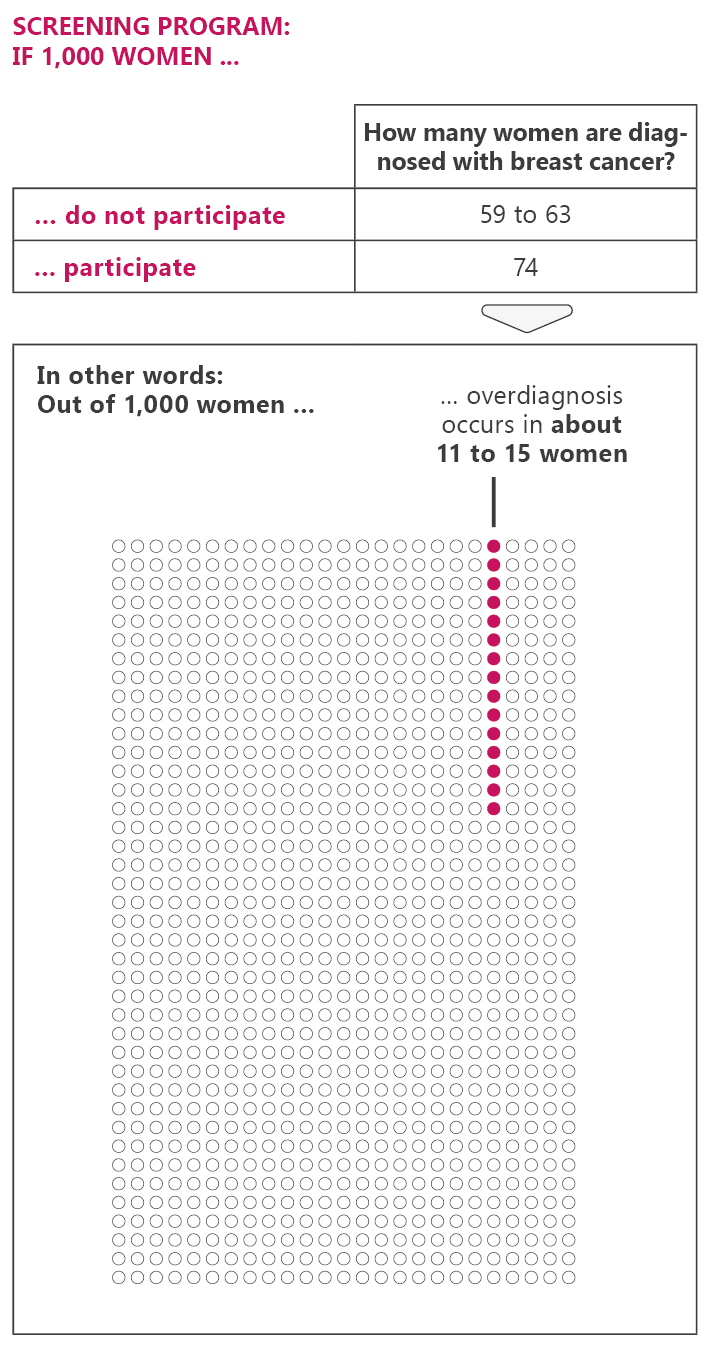
In Germany, women between the ages of 50 and 75 can have a free mammogram every two years. This option ends on their 76th birthday. The screening aims to detect breast cancer as soon as possible in order to provide better treatment and increase the chances of recovery. But mammograms can have drawbacks too. For instance, they may lead to unnecessary treatment.
In screening programs, everyone in a certain group (for instance, a certain age group) is offered a specific screening test. The cost of mammograms for breast cancer screening are covered by statutory health insurers. If you have private health insurance, it’s best to check if your insurer will cover these costs.
Women between the ages of 50 and 75 receive a letter from their mammography program center (Zentrale Stelle) every two years, inviting them to have a mammogram. The letter includes a suggested appointment time and date, as well as decision aid. The women can decide themselves whether or not they would like to have a mammogram.