Early-stage breast cancer: Does it make sense to have chemotherapy?

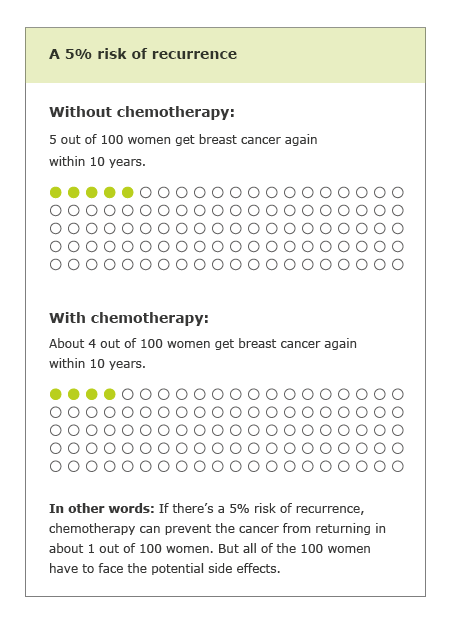
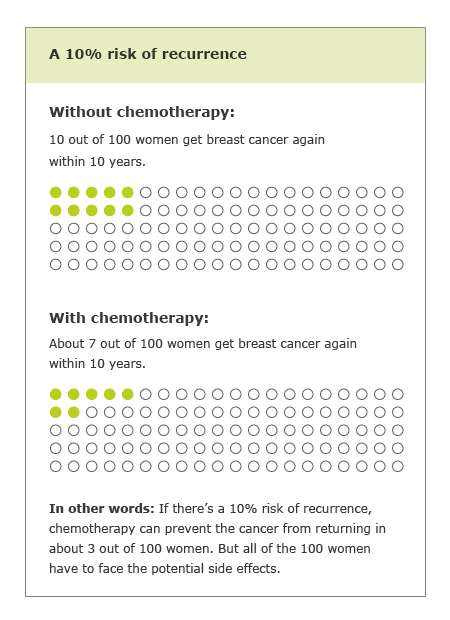
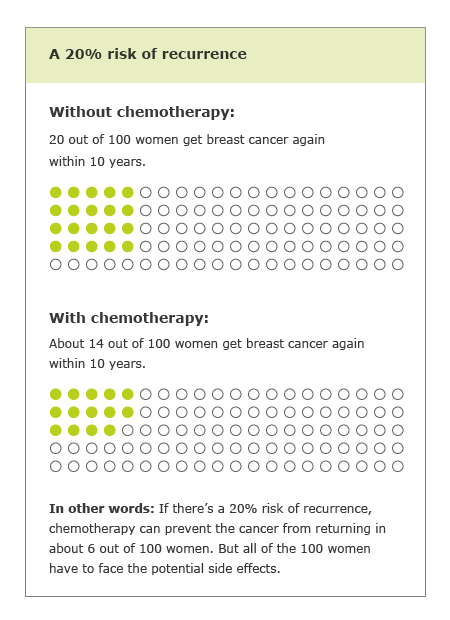
Women who have had surgery to remove early-stage breast cancer are often worried that the cancer will return. Chemotherapy can reduce the likelihood of a recurrence. But this treatment isn’t always a good idea because the disadvantages sometimes outweigh the advantages.
If breast cancer is discovered at an early stage, surgery can often remove all of the tumor. Many women have radiotherapy too. But some cancer cells might be left in the body. These can start growing again after a while, even years later. The medical term for this is “recurrence” or “relapse.”
The tumor may grow back in the breast or in nearby tissue (a local recurrence) or spread to a different part of the body (distant recurrence). If breast cancer comes back, the chances of a full recovery are usually much lower.
When deciding about treatment, it’s important to know how high the risk of recurrence is: The higher the risk, the greater the potential benefit of chemotherapy. Because of this, doctors routinely determine the risk of recurrence after breast cancer surgery.