Treatment for lymphedema is usually made up of several elements: compression therapy, lymphatic drainage, exercises and skin care. Taking a combined treatment approach can help make the swelling go down and relieve the other symptoms.
Compression therapy: Compression bandages or "sleeves" are used to put light pressure on the arm, which makes it easier for the lymph vessels to drain lymph fluid. They are worn during the day and then taken off at night, but some people also leave them on overnight.
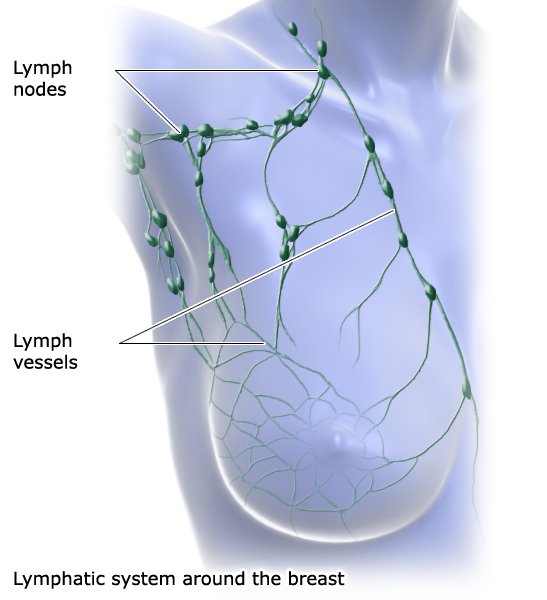
Lymphatic drainage: This is a type of massage that aims to help drain the trapped lymph fluid out of the body tissue. A physical therapist gently stimulates the tissue by moving their palms in gentle, circular motions.
Exercises: A program with suitable exercises is individually tailored to a person’s needs, and a physiotherapist also monitors the effects of the exercises. In the past, women were generally advised to get plenty of rest after breast cancer surgery. It was thought that exercise increases the risk of developing lymphedema. Studies have now shown that this is not the case.
Skin care: Lymphedema also affects the skin. So it is important to regularly care for your skin by applying moisturizers or lotions. Healthcare professionals can help you find suitable products.
When compression, exercise, lymphatic drainage and skin care is combined, there are hardly any side effects, and they are quite minor. Less than 1 out of 100 women have skin irritations, headaches or arm pain.
If the combined treatment doesn’t help enough, compression pumps can be used too.