Why is mechanical ventilation even needed during an operation?
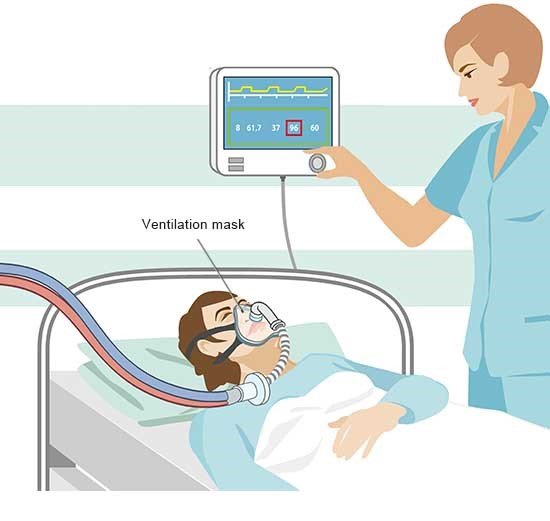
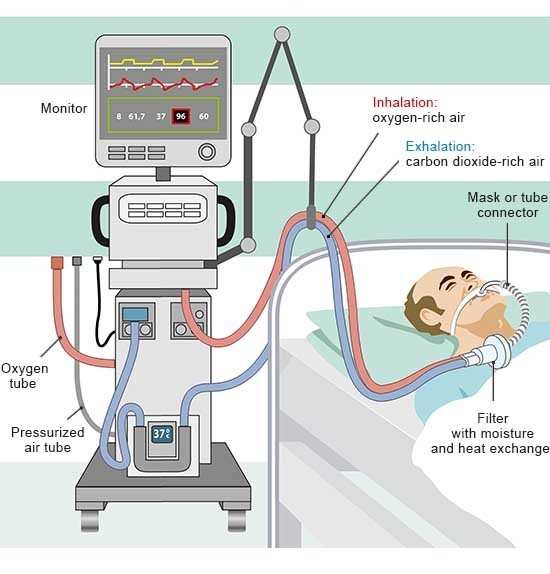
An anesthetic is necessary to make sure that a surgical procedure doesn't cause any pain. It is sometimes enough to just anesthetize (numb) one part of the body, such as the edges of a wound, only one arm, or the lower abdomen. However, a general anesthetic is usually needed for more extensive surgery. It deactivates our consciousness and the pain receptors in our body. Depending on how strong the anesthetic is, it can also stop our breathing. A ventilator then has to take over our breathing.