The knee is the joint that connects the bones of the upper and lower leg. It is needed for pretty much any form of movement – such as running, cycling or swimming. The knee is the body’s largest joint, and it has a fairly complex structure. This structure makes it possible for us to bend and straighten our knees, and to turn them slightly inward or outward.
A healthy knee can be moved from 0 degrees (completely straight) to about 150 degrees (calf touching the back of your thigh). A bent knee can be turned inward (towards the other leg) by about 10 degrees, and outward by about 30 degrees. A number of bones, muscles, and ligaments come together in the knee joint.
The bones of the knee
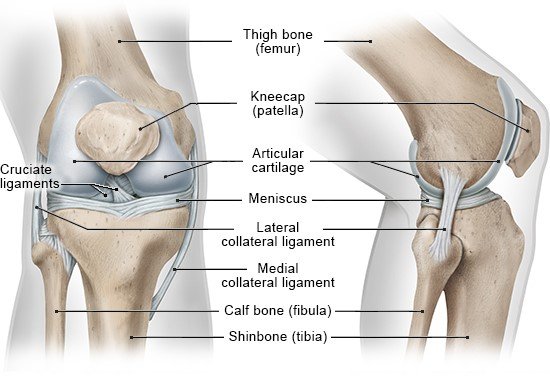
The knee joint is made up of three bones:
- Femur (thigh bone)
- Tibia (lower leg bone)
- Patella (kneecap)
There are two rounded joint surfaces, known as condyles, at the lower end of the femur (thigh bone). The cruciate ligaments run through the gap between these two projections.
The femur’s condyles are located opposite two relatively flat, slightly pan-shaped joint surfaces on the tibia (shinbone). There are two small bumps between them, to which the cruciate ligaments are attached.
The kneecap is located in front of the femur, above the condyles. It is connected to the tibia by the patellar tendon. When the knee is bent or straightened, the slightly wedge-shaped inner side of the kneecap, which is covered with articular (joint) cartilage, slides along a groove in the femur. The kneecap reduces the friction between the tendon and the bone, and it keeps the tendon from slipping sideways too. It also extends the lever effect of the femur, improving the transfer of force.
The three parts of the knee joint
The three parts (compartments) of the knee joint are found where the joint surfaces of the femur, tibia, and the back of the kneecap meet:
- The joint between the femur and tibia on the inner side of the knee (medial compartment)
- The joint between the femur and tibia on the outer side of the knee (lateral compartment)
- The joint between the kneecap and its groove on the femur (patellofemoral compartment)
All of the joint surfaces are covered with strong articular (joint) cartilage. Healthy cartilage provides a well-lubricated surface that allows smooth, low-friction movement between the bones.
The articular cartilage is 1 to 6 millimeters thick. There are no blood vessels in the cartilage. Instead, synovial fluid in the articular (joint) capsule supplies the cartilage tissue with nutrients. In order for the fluid to enter the cartilage and for waste substances to be transported out, the knee needs to be moved and bear weight. When pressure is put on the knee, the cartilage releases waste products. When the pressure is reduced, the cartilage absorbs nutrients from the fluid in the joint. So the knee has to be moved enough in order to keep the cartilage healthy.
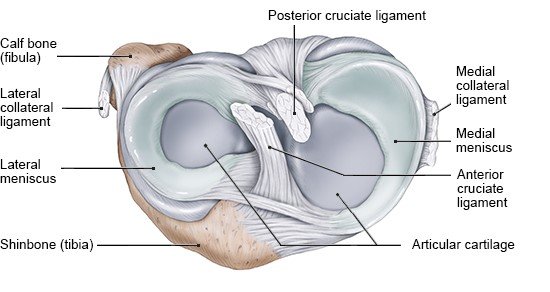
The meniscus
The two menisci (singular: meniscus) of the knee are located on the joint surfaces of the tibia. There is one medial (inner) meniscus and one lateral (outer) meniscus. These two half-moon-shaped pieces of fibrous cartilage are held in place by ligaments, in the middle of the knee. The outer sides of the menisci are attached to the joint capsule, and the medial meniscus is also attached to the medial collateral ligament.
The condyles of the femur rest directly on the tibia in the middle of the joint surfaces. The movable menisci are located between them on the outer edges. They make it possible to turn the knee a few degrees inward and outward.
If, for example, the knee is twisted or bent too fast during a fall, the menisci can become pinched between the condyles and rupture (tear).
Four ligaments give the joint stability
Two collateral (side) ligaments and two cruciate ligaments provide the knee joint with support and protect it from being twisted:
- The medial collateral ligament connects the inner sides of the femur and tibia bones, and is also attached to the joint capsule.
- The lateral collateral ligament connects the outer sides of the femur and tibia bones. It is not attached to the joint capsule.
- The anterior cruciate ligament runs from the back of the outer condyle to the front of the tibia.
- The posterior cruciate ligament runs from the front of the inner condyle to the back of the tibia.
The medial and lateral collateral ligaments stabilize the knee when the leg is straight. The knee can hardly be turned or rotated at all in this position.
When the knee is bent, the medial and lateral collateral ligaments relax, and the cruciate ligaments help to support it. When the knee is turned inwards, the cruciate ligaments wrap around each other to stabilize the joint in the direction it’s turned in.
Accidents, for instance while skiing or playing soccer, can cause the ligaments to tear. That can result in severe pain and swelling, and abnormal flexibility of the joint in certain directions – depending on which ligaments have been damaged.
The muscles and tendons allow the knee to move
The knee can be bent, stretched and turned with the help of many muscles and tendons, which connect the muscles to the bones. The two main groups of muscles are:
- The quadriceps femoris on the front side of the thigh: It’s also known as the quadriceps extensor (quads) because it helps to extend the knee.
- The biceps femoris on the back of the thigh: Together with other muscles, it makes it possible to bend the knee.
Many other smaller muscles are responsible for turning the knee – such as the sartorius muscle and the popliteus muscle.
Lippert H. Lehrbuch Anatomie. München: Urban und Fischer; 2017.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Stay informed
Subscribe to our newsletter or newsfeed. You can find our growing collection of films on YouTube.