Lyme disease

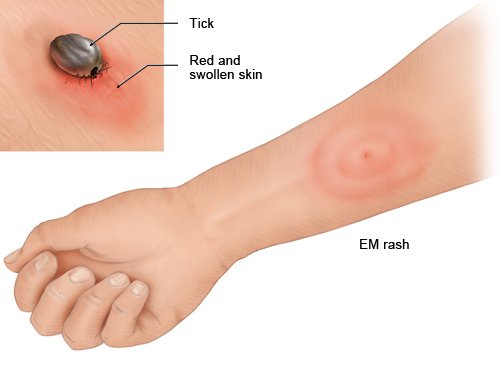
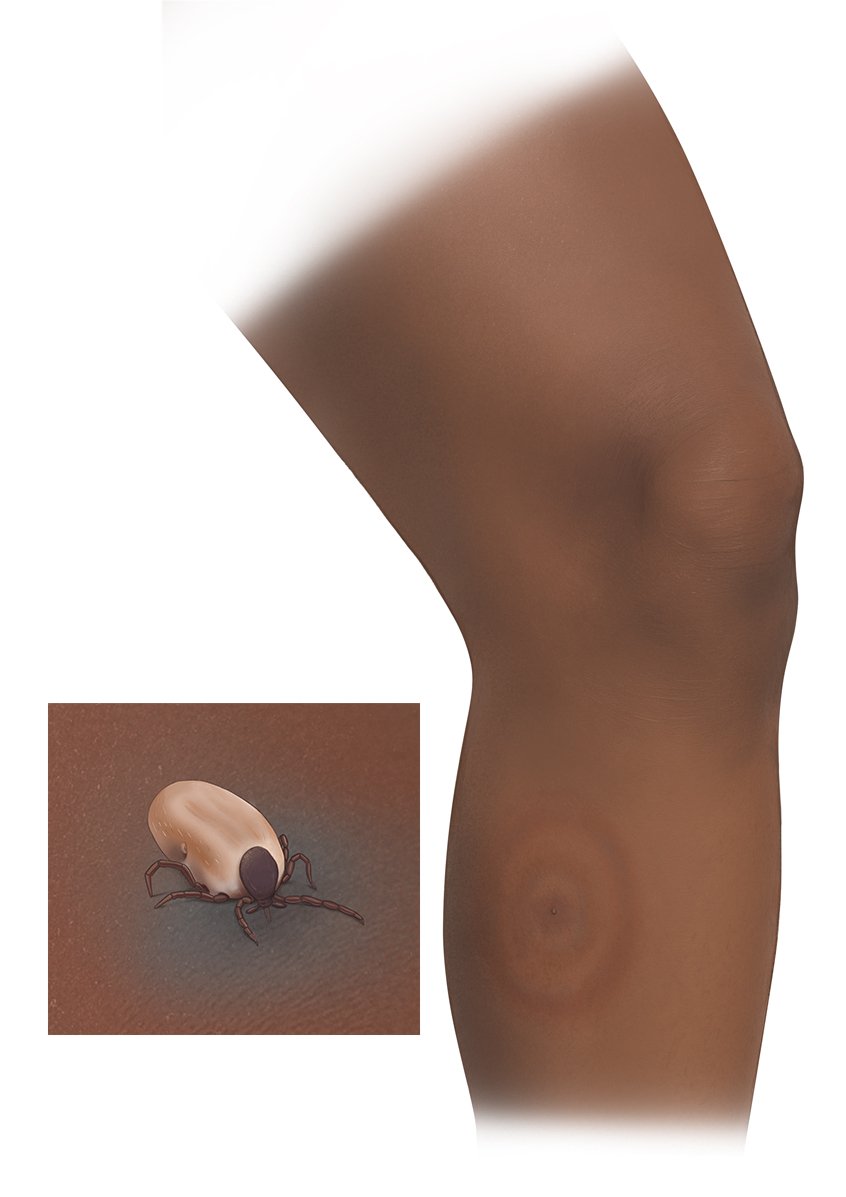
Some ticks carry Lyme disease, which can be transferred when they bite. One early symptom is circular redness forming around the tick bite. Lyme disease is usually treated with antibiotics. Complications may develop if it is left untreated. You can prevent infection by removing the tick in time.
Lyme disease is an infectious disease caused by bacteria. You can get infected if a tick bites you. Lyme disease is more common than tick-borne encephalitis (TBE), another disease that can be transmitted by ticks. In Germany, about 2 out of 10,000 people develop Lyme disease each year.