Introduction

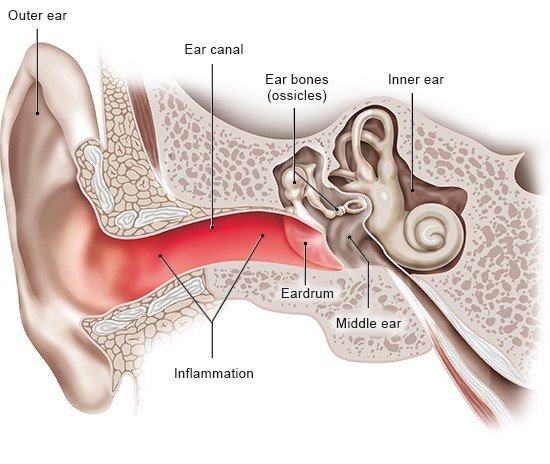
Outer ear infections typically lead to redness and swelling in the ear. They are among the most common causes of earache. In many cases they are caused by bacteria. But fungi, viruses or allergies are sometimes to blame too.
The outer ear includes the part of the ear you can see (the auricle) and the outer ear canal. The outer ear canal leads from the eardrum to the auricle. The medical term for inflammations of the outer ear is “otitis externa.” They are usually caused by infections.