Detecting melanoma

In order to detect melanoma skin cancer early on, you can either check your skin for abnormalities yourself or have a doctor examine it. Skin cancer can be treated more effectively if it is detected early on, before it spreads to other parts of the body.
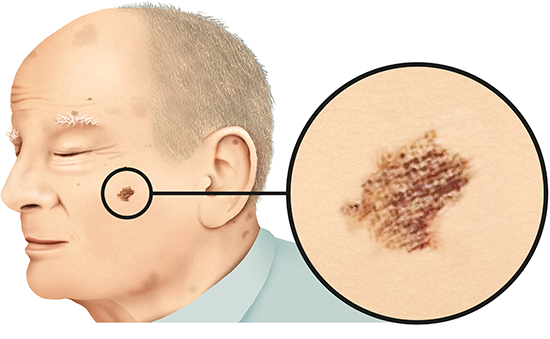
The older you get, the more your skin changes, and new moles or age spots (also known as liver spots or solar lentigines) may develop. This is a normal part of aging. So some people decide to wait and keep an eye on any unusual spots or patches of skin. Others want to know right away if something is wrong, and go to a doctor to have it checked out. But it is only rarely a serious disease like cancer.
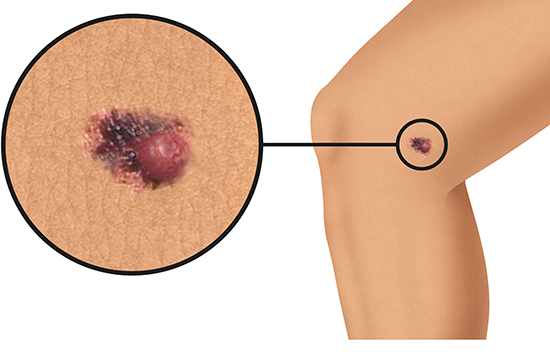
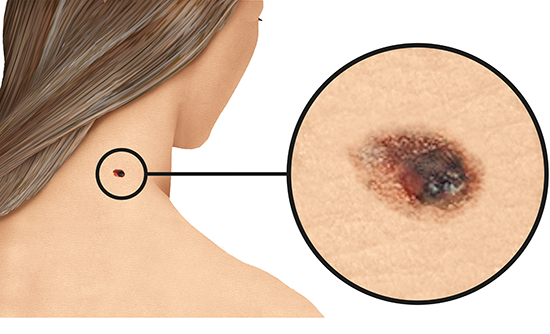
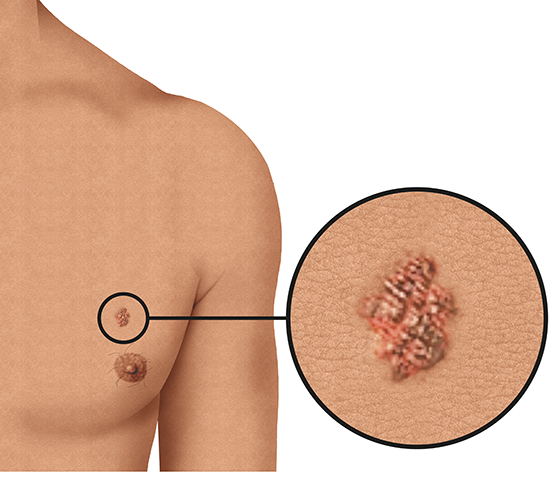
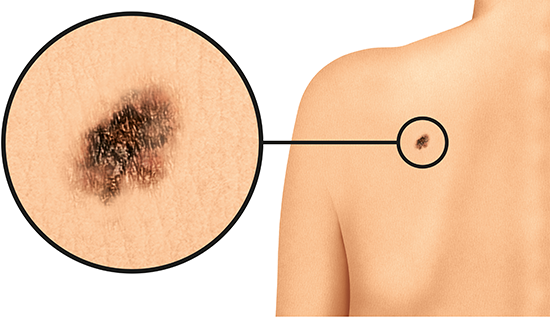
People who have been diagnosed with melanoma say that the affected spot or patch of skin changed in size, shape or color before. Carefully checking your skin on a regular basis is a good way to notice any changes.
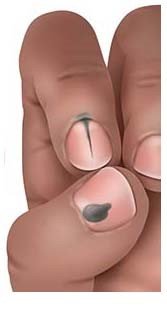
A full-body check involves inspecting every square inch of your skin, including the skin between your toes, on the soles of your feet, your ears, scalp, back, bottom and in your genital area. When checking parts of your body that are hard for you to see, it can be helpful to use a mirror or ask someone to help. That can be useful when checking your scalp, too – especially if you have very thick hair. Noting down the size of abnormal areas of skin or taking photos can make it easier to see whether they've changed the next time you check (either together with your doctor or using a special app).
It may be difficult to know what kind of changes are dangerous. If you think that something on your skin might be abnormal, and if it doesn't go away within 4 to 8 weeks, it's best to see a doctor. It can be harder to recognize melanoma on dark skin or very dark skin than on lighter skin.