How is cervical cancer treated?

Cervical cancer can be treated with surgery, radiotherapy, chemotherapy or immunotherapy. The choice of treatment will depend on various factors, including the stage of cancer and whether you still want to get pregnant.
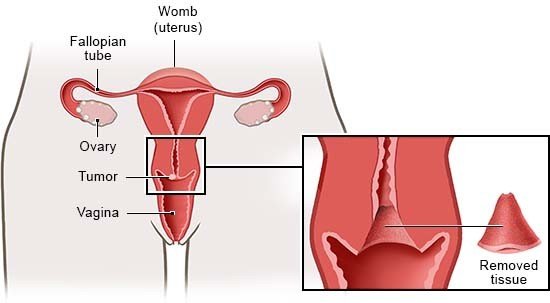
If cervical cancer is detected early on, it can often be removed completely with surgery. Then the chances of recovery are good. It is harder to treat if the cancer is already at a very advanced stage.
Experts recommend that cervical cancer be treated in specialized centers where different types of doctors work together – including gynecologists, oncologists, anesthesiologists, pathologists, radiologists and psycho-oncologists.