Surgery for diverticulitis and diverticular disease

Bowel surgery can sometimes relieve long-term symptoms caused by diverticula – but there are risks involved. Surgery is needed in some cases, though, to avoid serious diverticulitis-related complications such as an intestinal perforation (a hole in the wall of the bowel).
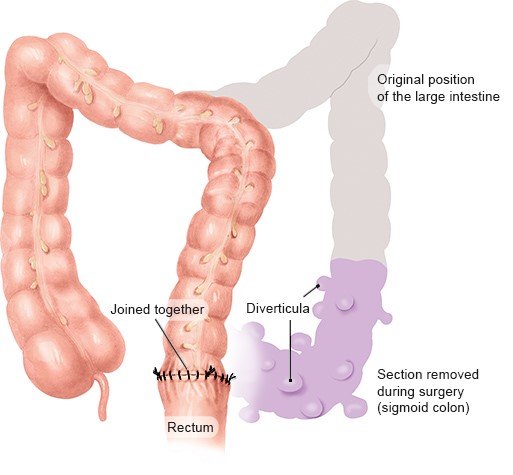
Diverticula are small pouches in the wall of the bowel, in which stool (poop) can get stuck. They are often harmless and do not cause any problems. If they do cause symptoms, they can usually be treated without surgery.
In non-emergency situations, it’s important to carefully consider the pros and cons of bowel surgery for diverticula-related problems before making a decision. This surgery is associated with risks, and there’s no guarantee that it will make the symptoms go away. Whether or not surgery is considered will depend on various factors, including the severity of the symptoms, how long you have had them, the risk of complications, and how effective other measures have been.