Introduction

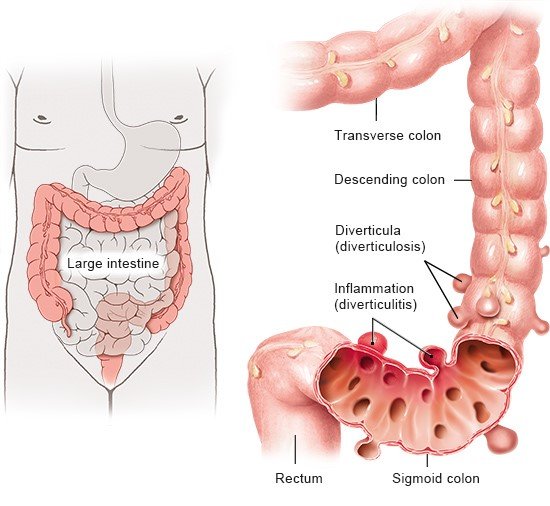
Symptoms like pain in the lower abdomen, flatulence, constipation and diarrhea may be caused by diverticula. Diverticula are pouches in the lining of the bowel (intestine). They arise when the wall of the bowel bulges out through weak areas of bowel muscle. The pouches are usually small and balloon-like, and the contents of the bowel (stool, or “poop”) might get into them. Diverticula are often harmless, but can lead to pain and other symptoms in the bowel or become infected.
Simply put, there are three different forms:
- Diverticulosis: You have diverticula, but no symptoms.
- Diverticular disease: This general term is used when the diverticula cause symptoms or complications. If the symptoms never really go away or keep coming back, it is considered to be chronic diverticular disease.
- Diverticulitis: The diverticula are inflamed or infected. This can lead to acute symptoms or chronic diverticular disease. If diverticulitis results in a collection of pus (an abscess), it's considered to be complicated diverticulitis. If not, it's known as uncomplicated diverticulitis.
Diverticulitis can usually be treated effectively, but may have serious consequences if an infection spreads.