How is acute diverticulitis treated?

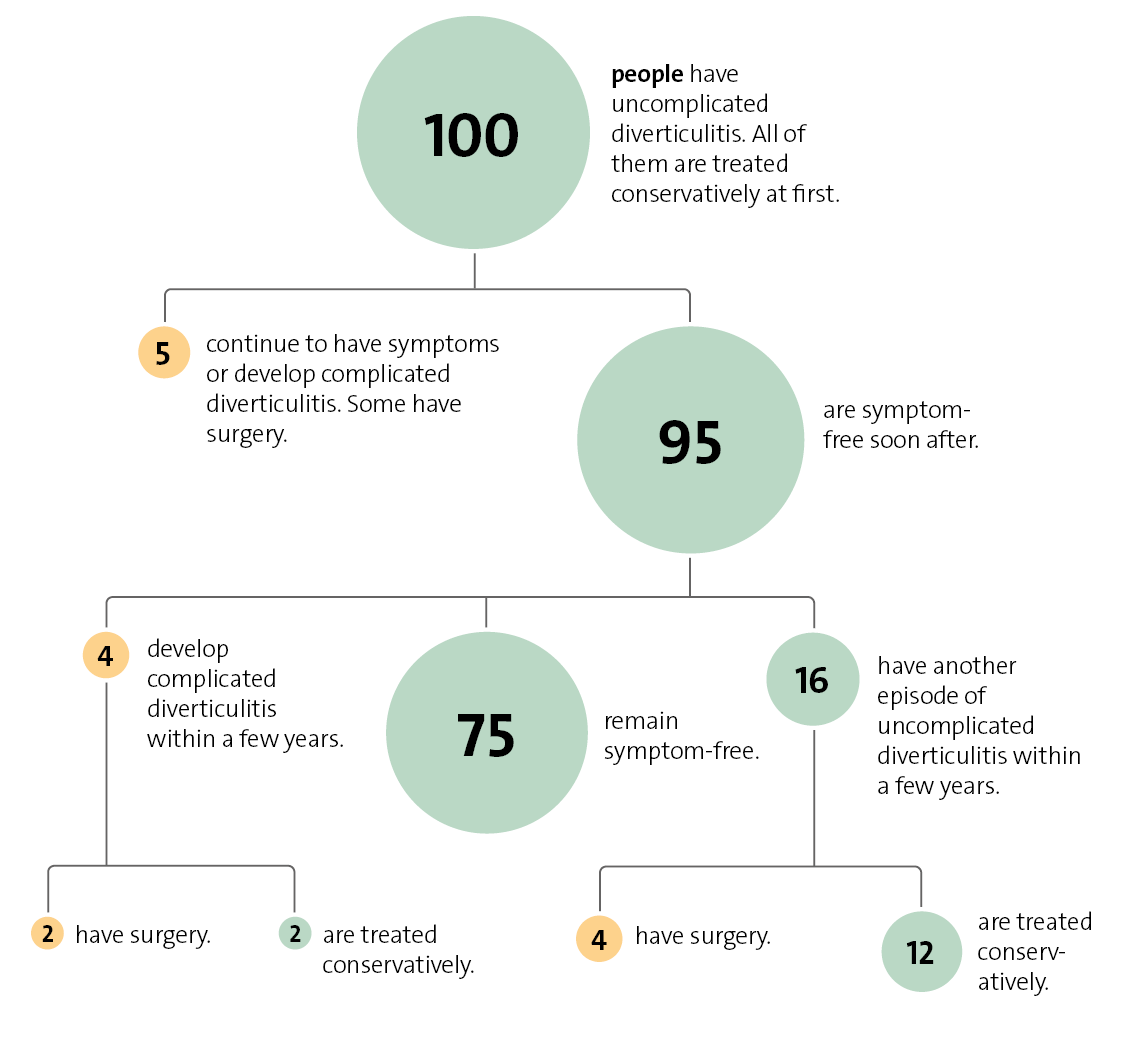
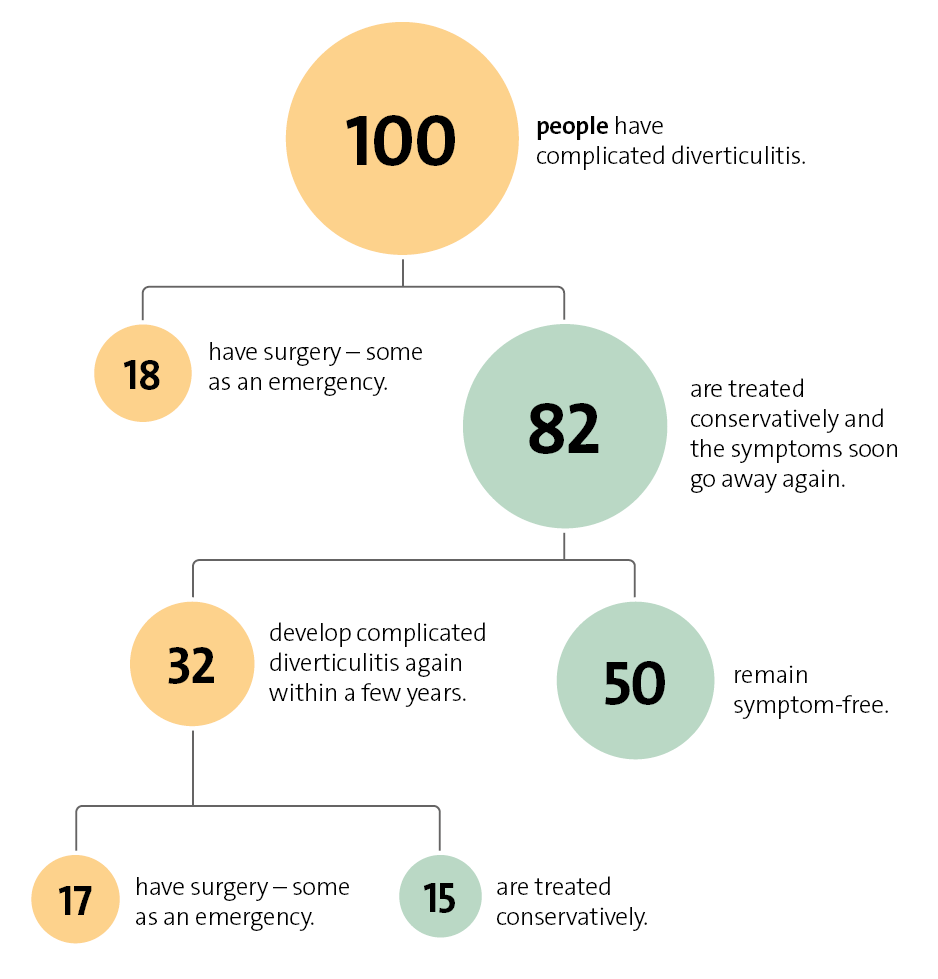
Uncomplicated diverticulitis usually goes away within a week – often without the need for treatment with antibiotics. But it's important to have regular check-ups to detect potential abscess-related complications early on. Complicated diverticulitis is usually treated with antibiotics. Surgery is sometimes needed.
Diverticula are small sac-like pouches in the wall of the bowel. They are often harmless and may go unnoticed. Sometimes one or more diverticula become inflamed or infected, leading to diverticulitis. This causes symptoms such as pain in the lower left part of the abdomen (belly), fever and digestive problems. There are two forms of diverticulitis:
- Uncomplicated diverticulitis: Diverticula and the surrounding lining of the bowel are inflamed or infected but there are no signs of pus building up (abscesses) or anything spreading. About 80% of people who have diverticulitis have the uncomplicated form.
- Complicated diverticulitis: Abscesses have developed. Sometimes the inflammation or infection has already spread or the wall of the bowel has torn (intestinal perforation). The bowel may also become blocked, or the membrane surrounding the organs in the belly may become inflamed (peritonitis). About 20% of people with diverticulitis have complicated diverticulitis.
Acute diverticulitis that has been successfully treated may come back again after some time. The risk of this happening is greater after having the complicated form.