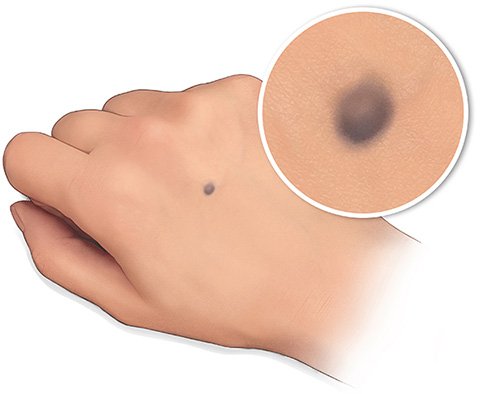
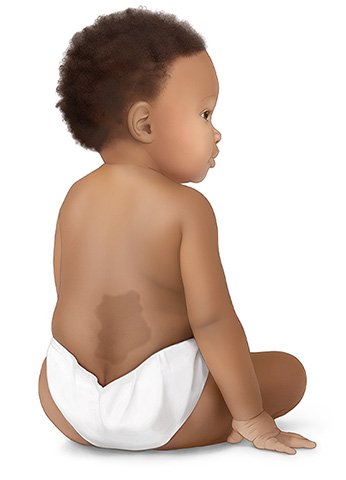
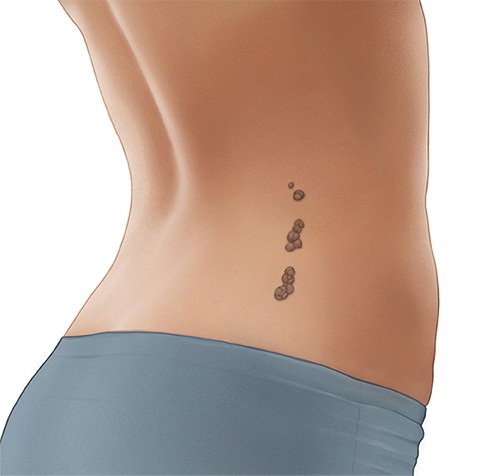
You can see moles, birthmarks and other nevi just by looking at your skin. If you want to know exactly what type of nevus you have, you can ask your doctor. People who go for skin cancer screening will have their nevi checked there, anyway. In Germany, statutory health insurers cover the costs of this screening every two years from the age of 35.
It is especially important to see a doctor if a nevus
- grows,
- changes shape or color,
- becomes crusty and scabs over,
- itches, or
- bleeds now and then without injury.
Changes like that could be a sign of skin cancer. You should also see a doctor soon if you have a nevus that looks very different to other nevi – perhaps because of an irregular shape, a jagged edge or raised areas – even if it hasn't changed.
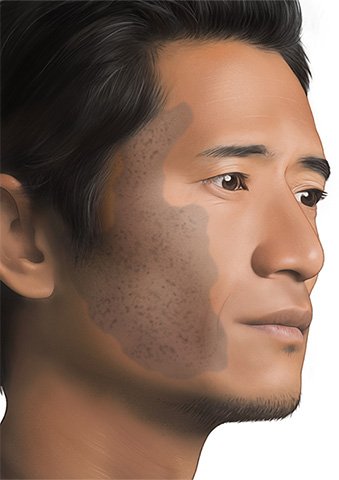
The doctor will take a very close look at the spot or area of skin and feel it with their hands. They will sometimes feel the surrounding areas of the body, too. Usually, they will take a close look at all of your skin during the examination. They will sometimes press a see-through glass spatula onto the nevus: If it fades, it has probably developed from blood vessels.
A special kind of magnifying glass called a dermatoscope is used to take a very close look at the surface of the nevi. Some dermatoscopes can also take pictures. That way, the doctor can see whether the nevus has changed during later examinations.
If a nevus is removed because of suspected cancer, the removed tissue is carefully examined under a microscope. Doctors can then see whether it really is cancer and, if so, whether all of the cancer cells have been removed.