What is overdiagnosis?
Overdiagnosis is the diagnosis of a medical condition that would never have caused any symptoms or problems. This kind of diagnosis can be harmful if it leads to psychological stress and unnecessary treatments.
Most people associate having an illness with feeling ill. In other words, having noticeable symptoms and perhaps going to the doctor because of those symptoms. The doctor may ask you questions and do tests to try to find out what is causing the symptoms. This leads to a diagnosis. Once a diagnosis has been made, a suitable treatment can be chosen.
Due to screening, the term “illness” also has another meaning: Screening tests are done in order to discover illnesses before they cause symptoms. Examples include mammograms for the detection of breast cancer or PSA tests for the detection of prostate cancer. The idea is that diagnosing the disease at an earlier stage will improve the chances of successful treatment. So screening aims to discover illnesses that you can’t feel yet but that will sooner or later become noticeable and start causing problems.
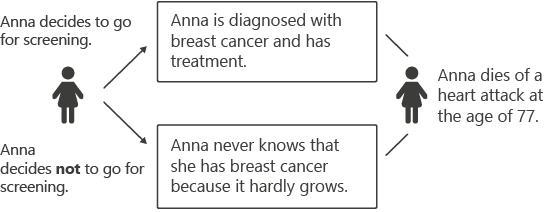
In recent decades it has become clearer that screening leads to the discovery of a different kind of “illness”: medical conditions that are “real” illnesses but would never cause any symptoms or problems, even without treatment.
Illnesses that never make you ill? That may not appear to make sense at first. Even medical professionals are only just starting to realize that this kind of diagnosis really exists. The medical term for the discovery of an illness that would never have caused any problems or led to death, even without treatment, is “overdiagnosis.”