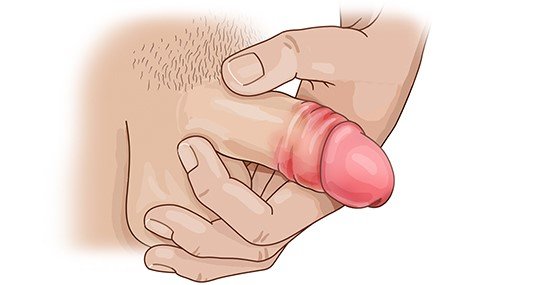
Carefully cleaning the inflamed area about 2 to 3 times a day (ideally using clear, lukewarm water) is usually enough to get rid of balanitis. You can dry the area with single-use cotton pads or dry cotton wipes from a pharmacy or drugstore.
You can try to speed up the healing process with compresses and sitz baths containing an antiseptic like octenidine, for example. Painkillers such as ibuprofen or acetaminophen (paracetamol) can be used if the pain is more severe.
If the symptoms don’t improve, it’s a good idea to see a doctor after one week at the latest. The doctor can then find the exact cause and recommend suitable products to apply to the affected area:
- Steroid creams and ointments can be used if the balanitis is caused by irritation or allergies.
- Antibiotic products are an option for bacterial infections.
- Antifungal products (antimycotics) are recommended for yeast infections.
These products are typically used until the inflammation has cleared up. But if the symptoms haven’t changed after 7 days or haven't completely gone away after 14 days, it’s a good idea to see your doctor again.
Important: Ointments and creams can damage latex condoms. Then the condoms no longer provide safe protection.
If the inflammation is caused by bacteria, your doctor might prescribe antibiotic tablets or an antibiotic syrup. These oral medications can also be used if it’s too difficult to apply creams to the glans and inside the foreskin because the foreskin is too tight. The tablets or syrup are usually taken for a week. Again, if the symptoms don’t improve despite the treatment, you should go back to your doctor.
If you keep getting balanitis because your foreskin is too tight, you can ask your doctor about the treatment options – like circumcision. But this surgical procedure can only be done once the inflammation has cleared up completely.
Balanitis rarely leads to complications. You should see a doctor if you develop any of the following symptoms:
- Fever, very severe pain or swollen lymph nodes in the groin.
- Swelling of the whole penis.
- Being unable to pee because of the inflammation. Urgent treatment is needed here.