Continuous glucose monitoring (CGM)
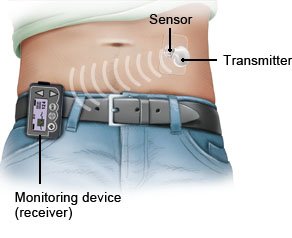
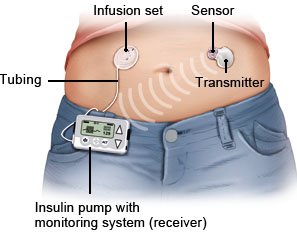
There are devices that regularly measure the levels of sugar in body tissue (continuous glucose monitoring, CGM). People who use a CGM device hardly need to prick their finger to measure their blood sugar levels anymore. These devices can also be used in combination with an insulin pump.
People who have type 1 diabetes need insulin injections every day. In rarer cases, some people with type 2 diabetes need them too. They either inject the insulin several times a day or are regularly supplied with insulin from an insulin pump.
In intensive insulin therapy, the amount of insulin used varies according to the body’s needs: A fixed amount of insulin is injected first to provide the body with a basic supply. Additional injections are given flexibly based on your blood sugar levels, the amount of food you eat and how physically active you are. So your sugar levels need to be measured several times a day. This can either be done using conventional blood glucose meters or a continuous glucose monitoring (CGM) system.