Is fibroid surgery a good idea?

Medication to treat fibroid symptoms usually only works while you are taking it. Many women who have heavy periods and severe pain end up considering surgery. There are a number of different types of surgical treatments, each with its own pros and cons.
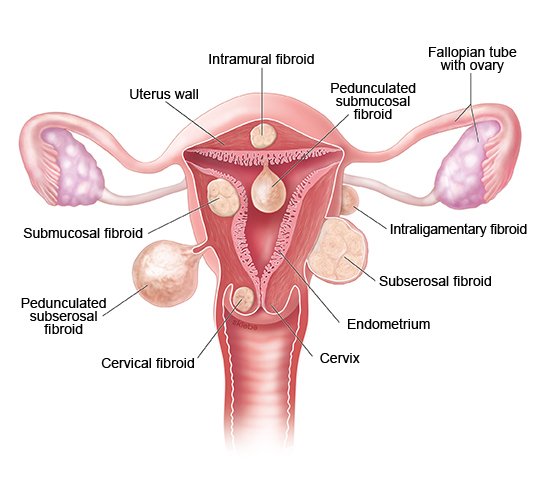
Surgery is done in the hope that it can permanently stop the symptoms of uterine fibroids. Some women do, in fact, experience long-term relief. But surgery always carries risks too. Whether or not surgery is an option – and, if so, what kind of surgery – will depend on how the woman feels about the different advantages and disadvantages. The size, number and location of the fibroids will also influence the choice of treatment. Not all types of surgery are suitable for women who still want to have children.
Your doctor may recommend taking hormones such as GnRH analogues for several months before having surgery. These kinds of artificial hormones are used to shrink the fibroids. Doctors can then make smaller cuts during surgery, allowing the womb (uterus) to recover more quickly. The drug ulipristal acetate is sometimes used for this purpose too.
But removing individual fibroids isn't a good idea if it might cause too much scarring in the womb, or if the risk of bleeding during or after surgery is too high. Plus, it isn't always absolutely certain that the symptoms will improve after surgery. Hysterectomy (surgical removal of the womb) is then an option – or possibly a non-surgical treatment approach such as uterine artery embolization (UAE, sometimes also called uterine fibroid embolization, or UFE). Uterine artery embolization cuts off the blood supply to the fibroid.