What different types of cardiac catheterization are there?
There are two main types of cardiac catheterization:
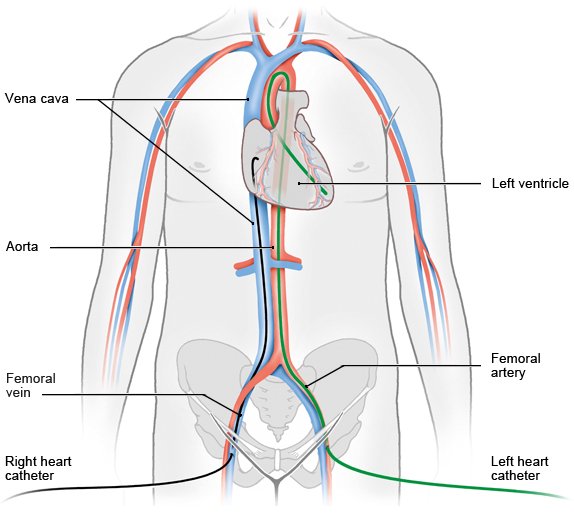
- Right heart catheterization (venous or flow-directed catheter): The catheter is inserted through a vein in the groin region or at the elbow and then advanced to the right ventricle and the pulmonary artery. Flow-directed catheters have a small inflatable balloon at the tip, allowing them to be carried by the flow of blood. The catheter is used to measure the pressure levels in the right ventricle and the pulmonary artery. A contrast medium is injected through the catheter so that the right chamber, the circulation of blood and the function of the cardiac valves can be examined.
- Left heart catheterization (arterial catheter): This catheter is advanced through an artery in your groin region, elbow or wrist and into the heart’s left ventricle. After a contrast medium has been injected it’s possible to examine the left ventricle, the aorta, the circulation of blood and the performance of the cardiac valves.