Introduction

Atrial flutter is a heart rhythm disorder that usually affects the right atrium of the heart and comes in attacks. It can develop if the heart is already damaged, for example by coronary artery disease.
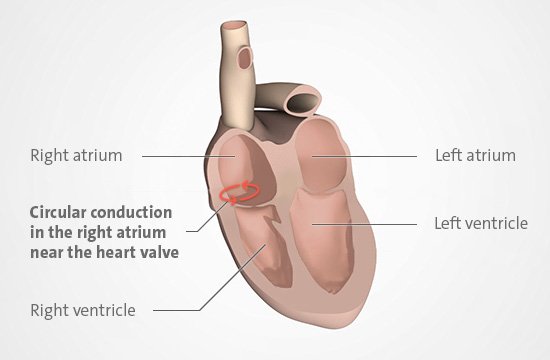
In atrial flutter, one of the electrical signals that makes the heart beat gets “stuck” in the right atrium and circles around there. That makes both atria beat very quickly – they “flutter.” As a result, the ventricles might also beat too quickly. As well as palpitations, this can cause dizziness, a tight feeling in the chest, and even short moments of unconsciousness.
Atrial flutter can have serious effects: Blood clots may form in the atria and cause a stroke. Atrial fibrillation is another possible effect. Unlike with atrial flutter, the atria don't beat more; they contract and “fibrillate.”
Atrial flutter often goes away by itself. If not, the heart’s normal rhythm can be restored with treatment using electricity (electrical cardioversion). Medication could be an option too. Surgery ( catheter ablation) can prevent atrial flutter from coming back.