Introduction

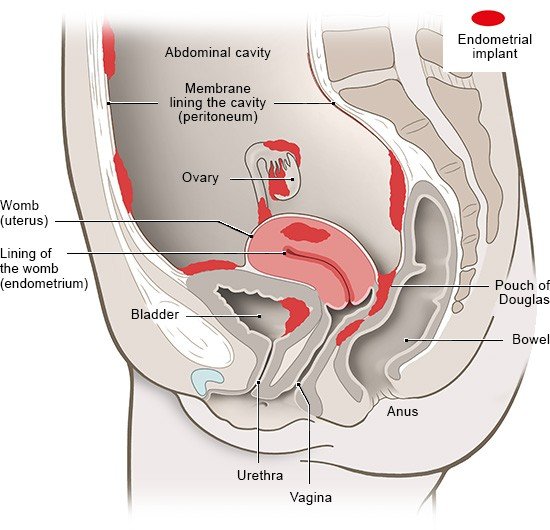
A lot of women think it's normal to have pain during their period – even excruciating pain – so they try to cope with it somehow. But severe period pain could be a sign of endometriosis. This chronic disease is one of the most common medical conditions affecting the abdomen (belly area) in women. In endometriosis, the kind of tissue that lines the womb (called the endometrium) is also found in the wall of the womb or elsewhere in the abdomen.
Known as “endometrial implants,” these areas of tissue don't cause any noticeable symptoms in many women. In others, though, they lead to severe pain or fertility problems. That can be very distressing, especially if your family or work colleagues don't take your issues seriously. It often takes years for endometriosis to be diagnosed as the cause of these problems.
There is currently no cure for endometriosis. But various things can be done to treat the symptoms. If the treatment is adapted to suit women’s personal circumstances, many can cope quite well with the disease. Getting hold of good information and working together with experienced, supportive doctors can help you to manage. But it's also important to get a feel for your body and know how it reacts to things.