How does ventilation therapy for respiratory problems work?
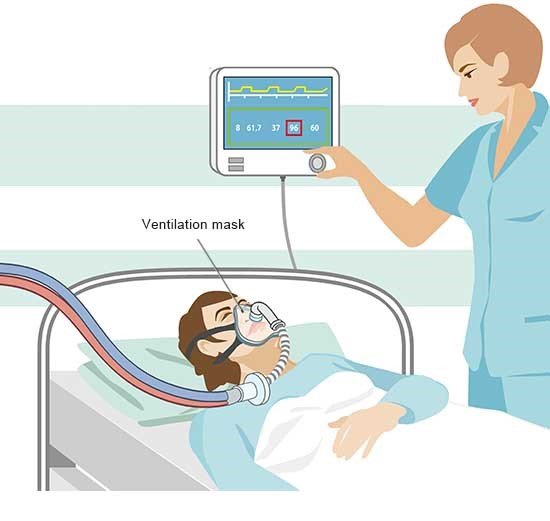
Ventilation therapy may be needed to treat lung disease, such as lung problems caused by severe pneumonia. But other illnesses such as nervous or muscular diseases can also cause breathing problems. Artificial ventilation is then sometimes needed.
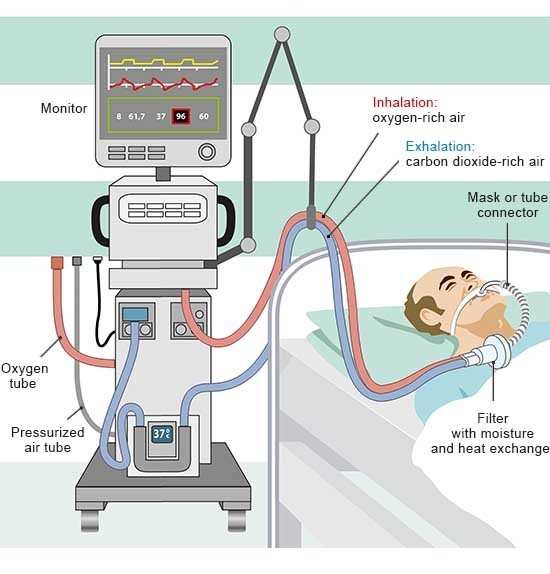
Ventilation therapy ensures that the body is provided with enough oxygen and allows excess carbon dioxide to leave the body. Unlike with first aid measures or operations under general anesthetic, this type of ventilation is usually performed for a longer period.