Medication for the treatment of fibromyalgia

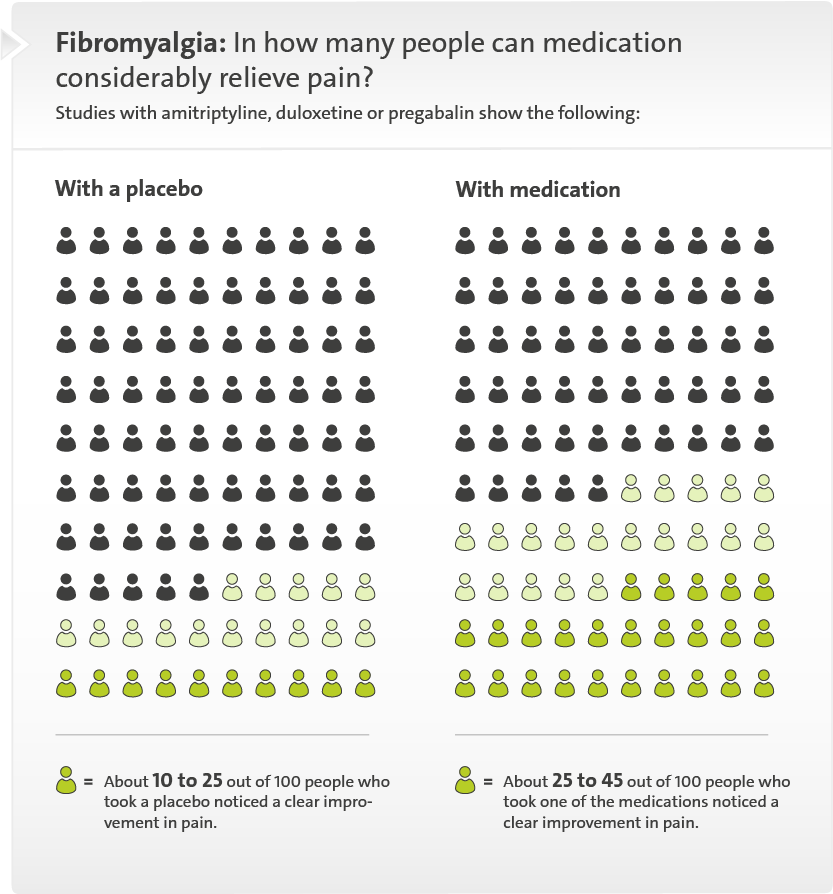
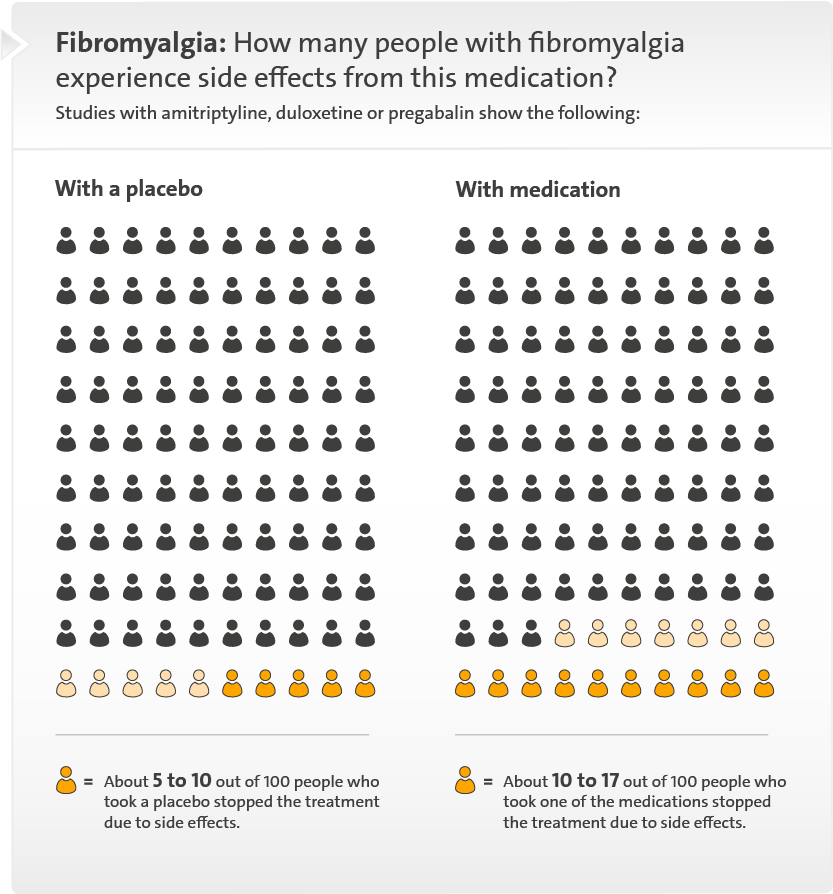
The drugs amitriptyline, duloxetine and pregabalin can relieve fibromyalgia pain in some people. They may cause side effects such as a dry mouth or nausea. Normal painkillers like ibuprofen or acetaminophen (paracetamol) aren’t recommended for the treatment of fibromyalgia.
There is currently no approved medication that was specifically developed for the treatment of fibromyalgia. But some medications that have been approved for the treatment of other types of chronic pain or diseases can help in fibromyalgia too. Studies have shown this to be true for the following drugs:
- amitriptyline
- duloxetine
- pregabalin
With the exception of amitriptyline, when these drugs are used for the treatment of fibromyalgia, it is legally considered to be unapproved (off-label) use. Special regulations apply here, affecting things like whether health insurers cover the costs. This is different if someone who has fibromyalgia also has a medical condition for which the medication has been approved, such as depression. It can take several weeks for the medication to start working.
It makes sense not to rely on medication alone, but instead combine it with other treatments. For instance, gentle physical exercise can relieve the symptoms and improve your resilience. The way you manage your life with the illness is important too – things like trying to reduce stress and planning your day to avoid overdoing it can help.