Overdiagnosis is the diagnosis of a medical condition that would never have caused any symptoms or problems. This kind of diagnosis can be harmful if it leads to psychological stress and unnecessary treatments.
Most people associate having an illness with feeling ill. In other words, having noticeable symptoms and perhaps going to the doctor because of those symptoms. The doctor may ask you questions and do tests to try to find out what is causing the symptoms. This leads to a diagnosis. Once a diagnosis has been made, a suitable treatment can be chosen.
Due to screening, the term “illness” also has another meaning: Screening tests are done in order to discover illnesses before they cause symptoms. Examples include mammograms for the detection of breast cancer or PSA tests for the detection of prostate cancer. The idea is that diagnosing the disease at an earlier stage will improve the chances of successful treatment. So screening aims to discover illnesses that you can’t feel yet but that will sooner or later become noticeable and start causing problems.
In recent decades it has become clearer that screening leads to the discovery of a different kind of “illness”: medical conditions that are “real” illnesses but would never cause any symptoms or problems, even without treatment.
Illnesses that never make you ill? That may not appear to make sense at first. Even medical professionals are only just starting to realize that this kind of diagnosis really exists. The medical term for the discovery of an illness that would never have caused any problems or led to death, even without treatment, is “overdiagnosis.”
What overdiagnosis doesn’t mean
It is important to know that overdiagnosis isn't the same as misdiagnosis. Misdiagnosis is a wrong diagnosis – for instance, if someone is diagnosed with cancer but they actually have a benign cyst. Overdiagnosis, on the other hand, is a “correct” medical diagnosis.
Overdiagnosis is also not the same as a false alarm. By this we mean abnormal findings, for instance seen in an x-ray, which further tests show to be harmless. The medical term for this is a false-positive result.
How do we know that overdiagnosis is an issue?
Most screening tests can lead to cases of overdiagnosis. This is well documented in the area of breast cancer screening and prostate cancer screening.
Studies on these two types of screening have shown that they can lead to overdiagnosis. The studies involved more than 10,000 women and men who were followed up for many years. Half of the participants were screened for cancer, and the other half weren't. Because the groups of participants were similar otherwise, you would expect a similar number of people in each group to develop cancer over time. The researchers kept track of how many people in the two groups developed cancer over a number of years, and compared the groups. The outcome: Considerably more people in the screening group were diagnosed with cancer. The studies on breast cancer screening, for instance, showed that about 2 out of 10 people who were diagnosed with breast cancer would never have noticed that they had a tumor if it hadn't been discovered through screening. The same may be true for up to 3 out of 10 people whose prostate cancer was discovered after they had a PSA test.
Why does overdiagnosis occur?
All screening tests can potentially result in overdiagnosis. This is of particular significance when it comes to cancer because a wide variety of cancer screening tests are offered. Also, it’s often impossible to accurately predict how a tumor will develop, especially in the early stages of cancer when it's small. Tumors don't always grow a lot and become life-threatening. They may develop in one of the following ways instead:
- The tumor may grow, but so slowly that the person dies of something else before the tumor starts causing symptoms.
- The tumor may not grow at all, or even disappear again on its own. Then the person may live a long life without ever knowing that they had cancer.
We know that some tumors don't grow, or only grow slowly, from studies in which autopsies were performed on elderly women and men who died of something else. For example, in some studies researchers took a very close look at the prostates of men who had died. The outcome: about 3 out of 10 men between the ages of 60 and 70 had a small prostate cancer tumor that they never knew about.
What are the consequences of overdiagnosis?
The consequences of overdiagnosis will largely depend on the medical condition in question: If screening leads to the discovery of a disease that doesn't appear to be very serious and is easy to treat, then overdiagnosis is harmless. But things are different if screening leads to the discovery of a disease like cancer. Then the diagnosis itself can already be very hard to cope with, having a major impact on your life.
If cancer is discovered through screening, it's generally impossible to know whether that person’s diagnosis is a case of overdiagnosis. So screening may lead to unnecessary treatments (“overtreatment”). Those treatments, such as surgery, are also distressing and sometimes associated with risks.
Overdiagnosis: An example
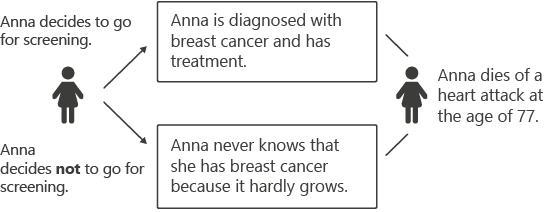
Picture a woman named Andrea. She is 65 years old and has a small, very slow-growing tumor in her breast. She doesn’t know about it. At the age of 77 she dies of a heart attack – not breast cancer.
If she had gone for screening at the age of 65, she would have been diagnosed with breast cancer and faced a lot of psychological stress and unpleasant treatments. She and her treatment team would then have believed that her tumor had been successfully “cured.” She wouldn’t actually have lived longer, though. But being a cancer patient would have greatly affected her wellbeing and quality of life.
What other kinds of screening can lead to overdiagnosis?
Overdiagnosis isn’t only an issue when it comes to cancer screening. Other examples include bulges in weak blood vessels (aneurysms) and abnormal-looking spinal discs. Some medical conditions are discovered purely by chance – for instance when doing tests for an unrelated medical problem. Routine check-ups may also lead to the discovery of abnormal readings or changes in tissue. It is hard to know how often we are “ill” and get better again without ever realizing it.
How can overdiagnosis be avoided?
Overdiagnosis would be significantly less of a problem if we could accurately predict the course of the disease that is diagnosed. Despite researchers’ efforts, reliable predictions aren't yet possible. With some illnesses, though, people can decide to wait and see what happens rather than starting treatment. For instance, after being thoroughly informed, some men with early-stage prostate cancer are prepared not to start treatment, and instead wait and see whether or how their tumor develops in the months and years that follow.
People who would like to avoid overdiagnosis at all costs would also have to avoid all types of screening.
Because some screening tests also have benefits, it’s worth finding out all about the screening test you are considering, and carefully thinking about the pros and cons. You may end up deciding to have one screening test, but not another. Screening tests are never urgent. There’s always enough time to get hold of information and think things over.
Making a decision
One important aspect is whether the screening test has even been proven to have any positive effects. Many of the screening tests offered in doctors’ practices and hospitals haven’t been proven to do so. So people who decide to have those screening tests enter risks without knowing whether there are any benefits.
Carefully considering the benefits and drawbacks of screening tests can help you reach the best decision for you:
- Would you rather have regular screening tests, even if that means risking overdiagnosis, with all the physical and psychological consequences?
- Or would you prefer to avoid unnecessary diagnoses and treatments – even if that means that a serious illness might only be discovered at a later stage, when treatment may be less effective?
Many people find it hard to make this kind of decision. It is important to carefully consider the pros and cons. Talk things over with the people you are close to, and don't hesitate to ask other doctors about the potential advantages and disadvantages of the screening test.
Bulliard JL, Chiolero A. Screening and overdiagnosis: public health implications. Public Health Rev 2015; 36: 8.
Carter SM, Rogers W, Heath I et al. The challenge of overdiagnosis begins with its definition. BMJ 2015; 350: h869.
Heath I. Role of fear in overdiagnosis and overtreatment - an essay by Iona Heath. BMJ 2014; 349: g6123.
Moynihan R, Doust J, Henry D. Preventing overdiagnosis: how to stop harming the healthy. BMJ 2012; 344: e3502.
Vaccarella S, Franceschi S, Bray F et al. Worldwide Thyroid-Cancer Epidemic? The Increasing Impact of Overdiagnosis. N Engl J Med 2016; 375(7): 614-617.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst 2010; 102(9): 605-613.
Welch HG, Schwartz LM, Woloshin S. Overdiagnosed: Making People Sick in the Pursuit of Health. Boston: Beacon Press; 2011.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Stay informed
Subscribe to our newsletter or newsfeed. You can find our growing collection of films on YouTube.