Anderson LJ, Nuckols TK, Coles C et al. A systematic overview of systematic reviews evaluating medication adherence interventions. Am J Health Syst Pharm 2020; 77(2): 138-147.
Armitage LC, Kassavou A, Sutton S. Do mobile device apps designed to support medication adherence demonstrate efficacy? A systematic review of randomised controlled trials, with meta-analysis. BMJ Open 2020; 10(1): e032045.
Boeni F, Spinatsch E, Suter K et al. Effect of drug reminder packaging on medication adherence: a systematic review revealing research gaps. Syst Rev 2014; 3: 29.
Chan A, De Simoni A, Wileman V et al. Digital interventions to improve adherence to maintenance medication in asthma. Cochrane Database Syst Rev 2022; (6): CD013030.
Chan AH, Foot H, Pearce CJ et al. Effect of electronic adherence monitoring on adherence and outcomes in chronic conditions: A systematic review and meta-analysis. PLoS One 2022; 17(3): e0265715.
Easthall C, Song F, Bhattacharya D. A meta-analysis of cognitive-based behaviour change techniques as interventions to improve medication adherence. BMJ Open 2013; 3(8): e002749.
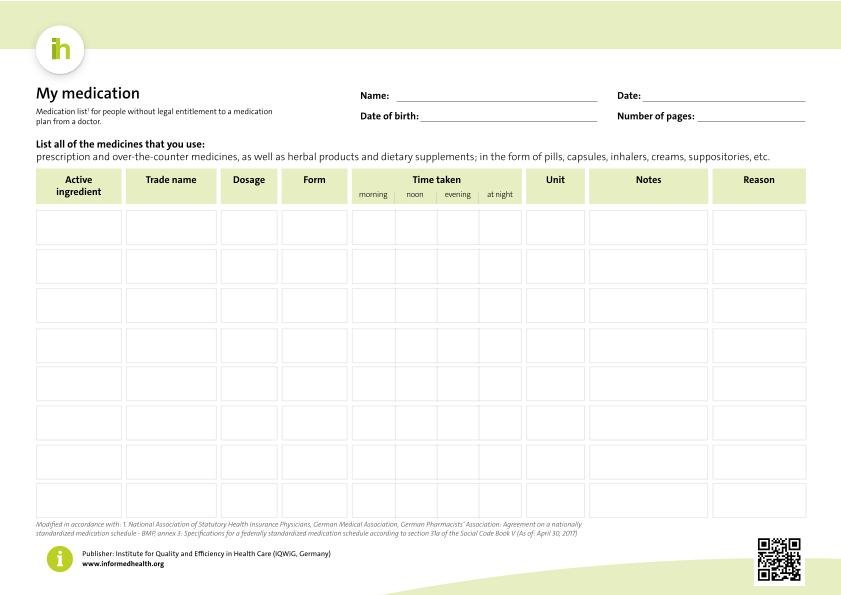
Kassenärztliche Bundesvereinigung (KBV). Ihr persönlicher Medikationsplan. Alle Medikamente auf einen Blick. 2021.
Mahtani KR, Heneghan CJ, Glasziou PP et al. Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database Syst Rev 2011; (9): CD005025.
Nieuwlaat R, Wilczynski N, Navarro T et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2014; (11): CD000011.
Palmer MJ, Machiyama K, Woodd S et al. Mobile phone-based interventions for improving adherence to medication prescribed for the primary prevention of cardiovascular disease in adults. Cochrane Database Syst Rev 2021; (3): CD012675.
Peng Y, Wang H, Fang Q et al. Effectiveness of Mobile Applications on Medication Adherence in Adults with Chronic Diseases: A Systematic Review and Meta-Analysis. J Manag Care Spec Pharm 2020; 26(4): 550-561.
Pound P, Britten N, Morgan M et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med 2005; 61(1): 133-155.
Redfern J, Tu Q, Hyun K et al. Mobile phone text messaging for medication adherence in secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2024; (3): CD011851.
Smith C, Gold J, Ngo TD et al. Mobile phone-based interventions for improving contraception use. Cochrane Database Syst Rev 2015; (6): CD011159.
Tan JP, Cheng KK, Siah RC. A systematic review and meta-analysis on the effectiveness of education on medication adherence for patients with hypertension, hyperlipidaemia and diabetes. J Adv Nurs 2019; 75(11): 2478-2494.
Tao D, Xie L, Wang T et al. A meta-analysis of the use of electronic reminders for patient adherence to medication in chronic disease care. J Telemed Telecare 2015; 21(1): 3-13.
Thakkar J, Kurup R, Laba TL et al. Mobile Telephone Text Messaging for Medication Adherence in Chronic Disease: A Meta-analysis. JAMA Intern Med 2016; 176(3): 340-349.
Vervloet M, Linn AJ, van Weert JC et al. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc 2012; 19(5): 696-704.
Viswanathan M, Kahwati LC, Golin CE et al. Medication Therapy Management Interventions in Outpatient Settings. 2014.
Wilhelmsen NC, Eriksson T. Medication adherence interventions and outcomes: an overview of systematic reviews. Eur J Hosp Pharm 2019; 26(4): 187-192.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.