Anheyer D, Haller H, Barth J et al. Mindfulness-Based Stress Reduction for Treating Low Back Pain: A Systematic Review and Meta-analysis. Ann Intern Med 2017; 166(11): 799-807.
Chenot JF, Greitemann B, Kladny B et al. Nichtspezifischer Kreuzschmerz. Dtsch Arztebl Int 2017; 114(51-52): 883-890.
Chou R, Deyo R, Friedly J et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017; 166(7): 493-505.
Hartvigsen J, Hancock MJ, Kongsted A et al. What low back pain is and why we need to pay attention. Lancet 2018; 391(10137): 2356-2367.
Hayden JA, Ellis J, Ogilvie R et al. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev 2021; (9): CD009790.
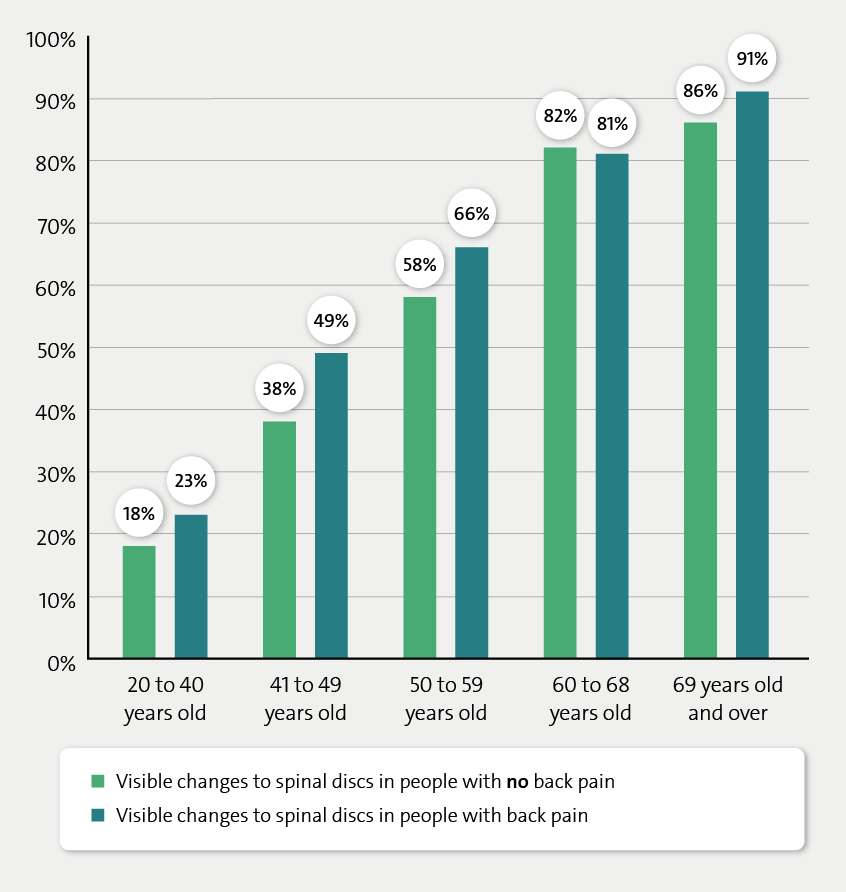
Kasch R, Truthmann J, Hancock MJ et al. Association of Lumbar MRI Findings with Current and Future Back Pain in a Population-based Cohort Study. Spine (Phila Pa 1976) 2022; 47(3): 201-211.
National Institute for Health and Care Excellence (NICE). Low Back Pain and Sciatica in Over 16s: Assessment and Management. 2016.
Pocovi NC, de Campos TF, Christine Lin CW et al. Walking, Cycling, and Swimming for Nonspecific Low Back Pain: A Systematic Review With Meta-analysis. J Orthop Sports Phys Ther 2022; 52(2): 85-99.
Pocovi NC, Lin CC, French SD et al. Effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention for the prevention of low back pain recurrence in Australia (WalkBack): a randomised controlled trial. Lancet 2024; 404(10448): 134-144.
Skelly AC, Chou R, Dettori JR et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. (AHRQ Comparative Effectiveness Reviews; No. 227). 2020.
Steffens D, Maher CG, Pereira LS et al. Prevention of Low Back Pain: A Systematic Review and Meta-analysis. JAMA Intern Med 2016; 176(2): 199-208.
Van der Gaag WH, Roelofs PD, Enthoven WT et al. Non-steroidal anti-inflammatory drugs for acute low back pain. Cochrane Database Syst Rev 2020; (4): CD013581.
Wallwork SB, Braithwaite FA, O'Keeffe M et al. The clinical course of acute, subacute and persistent low back pain: a systematic review and meta-analysis. CMAJ 2024; 196(2): E29-E46.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.